Helpful videos to guide your NF1-PN journey with GOMEKLI
Actor portrayal.
Talking to your doctor about GOMEKLI
Learn some tips on how to start a conversation with your doctor about GOMEKLI.
Petal shape from GOMEKLI logo appears onscreen, spinning as if the video is loading. Petal shape comes to a stop as full GOMEKLI logo fades in.
Image onscreen:
GOMEKLI logo shrinks and moves to top center of the frame. Indication statement appears.
Text onscreen and voice-over:
GOMEKLI (mirdametinib) is a prescription medicine used to treat adults and children 2 years of age and older with neurofibromatosis type 1 (NF1) who have plexiform neurofibromas (PN) that cause symptoms and cannot be completely removed by surgery.
It is not known if GOMEKLI is safe and effective in children under 2 years of age.
Please see Important Safety Information later in this video and Patient Information available on GOMEKLI.com.
Image onscreen:
Screen fades to white and the video title appears. Flag with the logo in the top right corner of the frame appears, where it remains for the entirety of the video.
Text onscreen:
Talking to your doctor about GOMEKLI
Voice-over:
It can be hard to start a conversation about treatment or know what questions to ask. In this video, we’ll share some tips for having a productive conversation with your doctor.
Image onscreen:
A split screen of 2 individuals with NF1-PN is shown: On the left-hand side of the screen, a woman looks at herself in the bathroom mirror, and on the right side of the screen, a young boy gets help with his backpack from his mother.
Voice-over:
If you’re living with or caring for someone who has NF1-PN, you know firsthand the impact plexiform neurofibromas can have.
Image onscreen:
The woman sits at a desk with her computer open to the GOMEKLI website. She has a pen and paper in hand and is getting ready to write down information.
Voice-over:
When you need to talk about it with your doctor, it helps to be prepared with questions or concerns.
Image onscreen:
The image zooms in on the treatment goals the adult woman has written for herself.
Voice-over:
First, think about your goals. What are the treatment goals you’d like to set with your doctor for yourself or the person you care for? What else is important to you?
Image onscreen:
The woman smiles as she reviews the treatment goals she wrote on her notepad.
Voice-over:
Knowing what you’re looking for can help you and your doctor come up with a treatment plan that works for you. If you’re not sure, you can ask your doctor what they think some goals could be and you can discuss them together.
Image onscreen:
As the symptom types are introduced, the screen splits into 3 sections. The left panel shows a young boy grimacing as he accidentally bumps a PN on his elbow against a door. In the middle panel is an adult woman changing how she walks due to pain from her PN, and the panel on the right shows an adult male looking in the mirror at a PN, located on his neck, that has grown larger.
Text onscreen:
Tell your doctor about all of your medical conditions before starting GOMEKLI.
Voice-over:
Next, think about any new or worsening symptoms you’d like to discuss. Are you or the person you care for experiencing pain, difficulty moving around, or visible changes to your plexiforms? Are there other symptoms you want to mention?
Image onscreen:
A woman is sitting at a desk. Her computer displays the GOMEKLI website’s Resources page, and she is in the process of downloading the Doctor Discussion Guide.
Voice-over:
The GOMEKLI Doctor Discussion Guide is a resource you can use to start a conversation that will help you find out if GOMEKLI is right for you. It’s available on GOMEKLI.com and you can download it, fill it out, and save it for your appointment.
Image onscreen:
An adult woman sits at her computer, reviewing the downloaded NF1 symptom-tracker form.
Voice-over:
It has a place to capture what symptoms you or the person you care for is experiencing, and to rate how much those symptoms are impacting daily life.
Image onscreen:
The woman is now scrolling through the guide. She is reading through the frequently asked questions portion of the document.
Voice-over:
Finally, think about questions you’d like to ask your doctor about GOMEKLI treatment. The discussion guide has a list of commonly asked questions, like: How can GOMEKLI help? How is this medicine taken? When can I expect to see results? What are the most common side effects of GOMEKLI?
Image onscreen:
The woman is scrolling to the bottom of the document where there is a blank space provided for patients who need or want to ask personalized questions about their experiences with NF1.
Voice-over:
There’s also space where you can write down any other questions you may have so you’re prepared for the conversation.
Image onscreen:
We see the woman from a side angle, looking at her computer screen.
Voice-over:
Remember, this is a chance for you to learn about a treatment that may help you or someone you care about. The more information you have, the better equipped you’ll be to take part in treatment decisions.
Image onscreen:
The woman sits across from her doctor as they engage in conversation.
Voice-over:
Taking an active role in the discussion and standing up for what you want can help you get the care you need.
Image onscreen:
The conversation between the woman and her doctor continues. The patient is happily nodding, and in the end looks toward the camera and smiles.
Voice-over:
We hope your next doctor’s visit is a productive one. Feel free to rewatch this video at any time and explore additional resources at GOMEKLI.com.
Text onscreen and voice-over:
Important Safety Information
Before taking GOMEKLI, tell your healthcare provider about all of your medical conditions, including if you:
- Have eye problems
- Have heart problems
-
Are pregnant or plan to become pregnant. GOMEKLI can harm your unborn
baby
Females who are able to become pregnant:- Your healthcare provider should check to see if you are pregnant before you begin treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 6 weeks after your last dose.
- Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 3 months after your last dose.
- Tell your healthcare provider right away if your female partner becomes pregnant or thinks she may be pregnant during treatment with GOMEKLI.
-
Are breastfeeding or plan to breastfeed. It is not known if GOMEKLI passes
into your breastmilk.
- Do not breastfeed during treatment with GOMEKLI and for 1 week after your last dose.
- Talk to your healthcare provider about the best way to feed your baby during this time.
How should I take GOMEKLI?
- Take GOMEKLI exactly as your healthcare provider tells you to take it. Your healthcare provider may change your dose, temporarily stop, or permanently stop treatment with GOMEKLI if you develop certain side effects.
- Take GOMEKLI twice a day, about 12 hours apart, for 21 days, followed by 7 days off treatment, to complete a 28-day treatment cycle. Your healthcare provider will decide how many treatment cycles are right for you.
- Take GOMEKLI with or without food.
- GOMEKLI comes in two different dosage forms, GOMEKLI capsules and GOMEKLI tablets for oral suspension. Your healthcare provider will decide the dosage form and dose of GOMEKLI that is right for you.
- If you take GOMEKLI capsules: Swallow each capsule whole with drinking water. If more than 1 capsule is required, swallow 1 capsule at a time. Do not open, break or chew the capsules.
-
If you take GOMEKLI tablets for oral suspension, either:
- Swallow each tablet for oral suspension whole with drinking water. If more than 1 tablet is required, swallow 1 tablet at a time. OR
- Disperse the tablets for oral suspension in drinking water to make a liquid (suspension) before you take or give GOMEKLI.
- If you miss a dose of GOMEKLI, skip the missed dose and take your next dose at your regularly scheduled time.
- If you vomit at any time after taking GOMEKLI, do not take an additional dose. Take your next dose at your regularly scheduled time.
What are the possible side effects of GOMEKLI?
GOMEKLI may cause serious side effects, including:
-
Eye problems. GOMEKLI may cause eye problems that can lead to blindness.
Your healthcare provider will check your vision before and during treatment
with GOMEKLI. Tell your healthcare provider right away if you get any of the
following signs or symptoms of eye problems:
- Blurred vision
- Loss of vision
- Other changes to your vision
-
Heart problems. GOMEKLI may lower the amount of blood pumped by your heart,
which is common in children during treatment with GOMEKLI and can also be
severe. Your healthcare provider will do tests before you start GOMEKLI
treatment, every 3 months during your first year of treatment, and then as
needed to make sure your heart is working properly. Tell your healthcare
provider right away if you get any of the following signs or symptoms of
heart problems:
- Coughing or wheezing
- Shortness of breath
- Swelling of your ankles and feet
- Tiredness
- Increased heart rate
-
Skin problems. Skin rashes are common with GOMEKLI in both adults and
children and can also be severe. GOMEKLI can also cause hair loss
(alopecia). Tell your healthcare provider if you develop any of the
following signs or symptoms of skin problems:
- Flat skin rash
- Raised bumps on the skin
- Skin bumps that look like acne
- Skin redness
- Itchy rash
- Peeling skin
- Diarrhea
- Nausea
- Muscle, joint, and bone pain
- Vomiting
- Tiredness
The most common side effects of GOMEKLI in adults include:
The most common side effects of GOMEKLI in children include:
- Diarrhea
- Muscle, joint, and bone pain
- Stomach (abdominal) pain
- Vomiting
- Headache
- Skin redness, swelling, or pain around the fingernails or toenails
- Nausea
GOMEKLI may cause fertility problems in females, which may affect your ability to have children. Talk to your healthcare provider if you have concerns about fertility.
These are not all of the possible side effects of GOMEKLI. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Please see full Prescribing Information, including Patient Information and Instructions for Use, available on GOMEKLI.com.
Text onscreen:
Thank you!
©2025 SpringWorks Therapeutics, Inc. All rights reserved. GOMEKLI is a registered trademark of SpringWorks Therapeutics, Inc. C_GOM_US_0434 8/25
Voice-over:
Thank you for watching, and remember: You’ve got this!
Tests you may need as you get going
Learn more about the tests you may need before and throughout GOMEKLI treatment.
Petal shape from GOMEKLI logo appears onscreen, spinning as if the video is loading. Petal shape comes to a stop as full GOMEKLI logo fades in.
Image onscreen:
GOMEKLI logo shrinks and moves to top center of the frame. Indication statement appears.
Text onscreen and voice-over:
GOMEKLI (mirdametinib) is a prescription medicine used to treat adults and children 2 years of age and older with neurofibromatosis type 1 (NF1) who have plexiform neurofibromas (PN) that cause symptoms and cannot be completely removed by surgery.
It is not known if GOMEKLI is safe and effective in children under 2 years of age.
Please see Important Safety Information later in this video and Patient Information available on GOMEKLI.com.
Text onscreen:
Tests you may need as you get going
Voice-over:
Today we’re going to discuss some steps you may need to take before starting treatment with GOMEKLI. It’s important to know that after your healthcare provider decides GOMEKLI may be a good fit for you, it may take some time before you can get started on treatment. First, you may need to take some tests.
Image onscreen:
A woman talking with her doctor about tests she may need.
Text onscreen:
Echocardiogram Eye exam Blood tests Pregnancy test
Voice-over:
Some people taking GOMEKLI experienced serious side effects including heart and eye problems. To make sure you’re a good candidate for GOMEKLI treatment, your healthcare provider will order an echocardiogram to take a look at your heart…
Image onscreen:
A man in an exam room getting an EKG.
Voice-over:
…as well as an eye exam to check your vision and the overall health of your eyes. To make sure you get the proper tests, inform your eye doctor that you have NF1-PN and are planning to start GOMEKLI, a MEK inhibitor. You should also let your doctor know about all of your medical conditions, including if you have a history of eye problems, heart problems, are pregnant or plan to become pregnant, or are breastfeeding or plan to breastfeed.
Image onscreen:
Woman stands with words popping up around her.
Voice-over:
You’ll also take blood tests to check your levels before you start GOMEKLI. Your healthcare provider will want you to do these tests regularly throughout your treatment too, so they can check for any changes.
Image onscreen:
A doctor’s lab that has a microscope and vial holders.
Voice-over:
GOMEKLI may cause fertility problems in females, which may affect your ability to have children. If you’re able to become pregnant, your healthcare provider should give you a pregnancy test before you begin treatment, as GOMEKLI can harm your unborn baby. Talk to your healthcare provider if you have concerns about fertility. If you’re able to become pregnant, your healthcare provider should give you a pregnancy test before you begin treatment, as GOMEKLI can harm your unborn baby. Talk to your healthcare provider if you have concerns about fertility.
Image onscreen:
A doctor giving a patient a blood test.
Text onscreen:
You should use effective birth control (contraception) during treatment with GOMEKLI and for 6 weeks after your last dose. Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with GOMEKLI.
Voice-over:
Remember, these tests may take some time to schedule and complete, but there are things you can do in the meantime to prepare for treatment. GOMEKLI.com has resources available that can help.
Image onscreen:
A man sitting at his desk looking at GOMEKLI.com.
Voice-over:
Additionally, once you’ve been prescribed GOMEKLI, you can enroll in SpringWorks CareConnections, a free, personalized patient support program. SpringWorks CareConnections can help you with insurance navigation and provide educational and emotional support throughout treatment. It may be helpful to sign up for the program as soon as your healthcare provider prescribes GOMEKLI. SpringWorks CareConnections may also help with eligible out-of-pocket costs for certain treatment-related tests, examinations, and/or specialty visits during treatment with GOMEKLI.
Text onscreen:
Terms and conditions apply. Reimbursement for eligible treatment-related costs are subject to annual benefit maximums. To receive the reimbursement of eligible treatment-related expenses, an Explanation of Benefits (EOB) form must be submitted, along with copies of receipts for any payments made in full, or your healthcare provider may submit an invoice for services rendered. Full terms and conditions are provided during the enrollment process and are available upon request by contacting SpringWorks CareConnections® at 844-CARES-55 (844-227-3755).
Image onscreen:
The man on his phone sitting down.
Text onscreen:
Call SpringWorks CareConnections® at 844-CARES-55 (844-227-3755), Monday – Friday,
8AM–10PM ET.
Voice-over:
To see how SpringWorks CareConnections can help you, call 844-227-3755 Monday through Friday, between 8 AM and 10 PM Eastern Time.
Text onscreen and voice-over:
Important Safety Information
Before taking GOMEKLI, tell your healthcare provider about all of your medical conditions, including if you:
- Have eye problems
- Have heart problems
-
Are pregnant or plan to become pregnant. GOMEKLI can harm your unborn baby
Females who are able to become pregnant:- Your healthcare provider should check to see if you are pregnant before you begin treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 6 weeks after your last dose.
- Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 3 months after your last dose.
- Tell your healthcare provider right away if your female partner becomes pregnant or thinks she may be pregnant during treatment with GOMEKLI.
-
Are breastfeeding or plan to breastfeed. It is not known if GOMEKLI passes into your breastmilk.
- Do not breastfeed during treatment with GOMEKLI and for 1 week after your last dose.
- Talk to your healthcare provider about the best way to feed your baby during this time.
How should I take GOMEKLI?
- Take GOMEKLI exactly as your healthcare provider tells you to take it. Your healthcare provider may change your dose, temporarily stop, or permanently stop treatment with GOMEKLI if you develop certain side effects.
- Take GOMEKLI twice a day, about 12 hours apart, for 21 days, followed by 7 days off treatment, to complete a 28-day treatment cycle. Your healthcare provider will decide how many treatment cycles are right for you.
- Take GOMEKLI with or without food.
- GOMEKLI comes in two different dosage forms, GOMEKLI capsules and GOMEKLI tablets for oral suspension. Your healthcare provider will decide the dosage form and dose of GOMEKLI that is right for you.
- If you take GOMEKLI capsules: Swallow each capsule whole with drinking water. If more than 1 capsule is required, swallow 1 capsule at a time. Do not open, break or chew the capsules.
-
If you take GOMEKLI tablets for oral suspension, either:
- Swallow each tablet for oral suspension whole with drinking water. If more than 1 tablet is required, swallow 1 tablet at a time. OR
- Disperse the tablets for oral suspension in drinking water to make a liquid (suspension) before you take or give GOMEKLI.
See the “Instructions for Use” that come with your medicine for instructions on how to prepare and take GOMEKLI tablets for oral suspension.
- If you miss a dose of GOMEKLI, skip the missed dose and take your next dose at your regularly scheduled time.
- If you vomit at any time after taking GOMEKLI, do not take an additional dose. Take your next dose at your regularly scheduled time.
What are the possible side effects of GOMEKLI?
GOMEKLI may cause serious side effects, including:
-
Eye problems. GOMEKLI may cause eye problems that can lead to blindness. Your healthcare provider will check your vision before and during treatment with GOMEKLI. Tell your healthcare provider right away if you get any of the following signs or symptoms of eye problems:
- Blurred vision
- Loss of vision
- Other changes to your vision
-
Heart problems. GOMEKLI may lower the amount of blood pumped by your heart, which is common in children during treatment with GOMEKLI and can also be severe. Your healthcare provider will do tests before you start GOMEKLI treatment, every 3 months during your first year of treatment, and then as needed to make sure your heart is working properly. Tell your healthcare provider right away if you get any of the following signs or symptoms of heart problems:
- Coughing or wheezing
- Shortness of breath
- Swelling of your ankles and feet
- Tiredness
- Increased heart rate
-
Skin problems. Skin rashes are common with GOMEKLI in both adults and children and can also be severe. GOMEKLI can also cause hair loss (alopecia). Tell your healthcare provider if you develop any of the following signs or symptoms of skin problems:
- Flat skin rash
- Raised bumps on the skin
- Skin bumps that look like acne
- Skin redness
- Itchy rash
- Peeling skin
The most common side effects of GOMEKLI in adults include:
- Diarrhea
- Nausea
- Muscle, joint, and bone pain
- Vomiting
- Tiredness
The most common side effects of GOMEKLI in children include:
- Diarrhea
- Muscle, joint, and bone pain
- Stomach (abdominal) pain
- Vomiting
- Headache
- Skin redness, swelling, or pain around the fingernails or toenails
- Nausea
GOMEKLI may cause fertility problems in females, which may affect your ability to have children. Talk to your healthcare provider if you have concerns about fertility.
These are not all of the possible side effects of GOMEKLI. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Please see full Prescribing Information, including Patient Information and Instructions for Use, available on GOMEKLI.com.
Text onscreen:
©2025 SpringWorks Therapeutics, Inc. All rights reserved. GOMEKLI and SpringWorks CareConnections are registered trademarks of SpringWorks Therapeutics, Inc. C_GOM_US_0392 11/25
Voice-over:
Thank you for watching. And remember: You’ve got this!
Support with SpringWorks CareConnections®
See all the different ways SpringWorks CareConnections can provide support throughout GOMEKLI treatment.
Petal shape from GOMEKLI logo appears onscreen, spinning as if the video is loading. Petal shape comes to a stop as full GOMEKLI logo fades in.
Image onscreen:
GOMEKLI logo shrinks and moves to top center of the frame. Indication statement appears.
Text onscreen and voice-over:
GOMEKLI (mirdametinib) is a prescription medicine used to treat adults and children 2 years of age and older with neurofibromatosis type 1 (NF1) who have plexiform neurofibromas (PN) that cause symptoms and cannot be completely removed by surgery.
It is not known if GOMEKLI is safe and effective in children under 2 years of age.
Please see Important Safety Information later in this video and Patient Information available on GOMEKLI.com.
Image onscreen:
Screen fades and the video title appears.
Text onscreen:
Support with SpringWorks CareConnections®
Voice-over:
Just getting started on GOMEKLI? In this video, we’ll explain how SpringWorks CareConnections can provide support throughout your treatment.
Image onscreen:
The SpringWorks CareConnections logo.
Voice-over:
SpringWorks CareConnections is a free, personalized patient support program for people taking GOMEKLI. The program is available throughout your treatment journey to help you navigate your insurance coverage, answer questions about your treatment, and help you start and stay on track with GOMEKLI.
Image onscreen:
A woman sitting at her computer while talking with a SpringWorks CareConnections Nurse Advocate.
Voice-over:
Enrollment only takes a few steps, and once you’re signed up one of our Nurse Advocates will give you a call to welcome you to the program. Your Nurse Advocate will be your single point of contact at SpringWorks CareConnections, and can provide you with personalized educational and emotional support. Some of the ways our Nurse Advocates can support you include helping you understand treatment with GOMEKLI, assisting you or your loved one with staying on track and taking the medication, and coordinating with your doctor’s office and pharmacy to make sure you receive GOMEKLI as prescribed. The SpringWorks CareConnections Patient Support Program is not intended to take the place of your healthcare provider, and our team of Nurse Advocates cannot provide medical or clinical advice.
Image onscreen:
A woman in her home thinking about the cost of treatment.
Text onscreen:
Terms and conditions apply. Copay program for GOMEKLI and reimbursement for eligible treatment-related costs are subject to annual benefit maximums. To receive reimbursement of eligible treatment-related expenses, an Explanation of Benefits (EOB) form must be submitted, along with copies of receipts for any payments made in full, or your healthcare provider may submit an invoice for services rendered. Full terms and conditions are provided during the enrollment process and are available upon request by contacting SpringWorks CareConnections® at 844-CARES-55 (844-227-3755).
Voice-over:
At SpringWorks, we don’t want concerns about cost or insurance coverage to come between you and your medication. The GOMEKLI Commercial Copay Program may be able to help you save. If you have commercial health insurance, our program could help you pay as little as a $0 copay per 21-day supply of GOMEKLI.
Image onscreen:
The woman pulling her SpringWorks CareConnections copay card from her wallet.
Voice-over:
It may also help with eligible out-of-pocket costs for certain treatment-related tests, exams, or specialty visits during treatment with GOMEKLI.
Image onscreen:
The Nurse Advocate and woman talking to each other.
Text onscreen:
Terms and conditions apply. PAP eligibility criteria and annual household income limits apply. Full terms and conditions are provided during the enrollment process and are available upon request by contacting SpringWorks CareConnections® at 844-CARES-55 (844–227–3755).
Voice-over:
And if you’re uninsured, lack coverage for GOMEKLI, or are experiencing financial hardship, ask your Nurse Advocate about the Patient Assistance Program, which may help you obtain GOMEKLI at no cost.
Image onscreen:
A woman enrolling in SpringWorks CareConnections.
Text onscreen:
Enroll in SpringWorks CareConnections® now!
Voice-over:
If you’re ready to start taking advantage of the support offered by SpringWorks CareConnections, you can enroll now by heading to the Savings & Support page of the GOMEKLI website and selecting the “Enroll now” button.
Text onscreen:
The SpringWorks CareConnections® Patient Support Program is not intended to take the place of your healthcare provider, and our team of Nurse Advocates cannot provide medical or clinical advice.
Voice-over:
At SpringWorks, we want to make sure that everybody taking GOMEKLI has access to support. We can’t wait to meet you and help you stay on track with your GOMEKLI treatment.
Text onscreen and voice-over:
Important Safety Information
Before taking GOMEKLI, tell your healthcare provider about all of your medical conditions, including if you:
- Have eye problems
- Have heart problems
-
Are pregnant or plan to become pregnant. GOMEKLI can harm your unborn baby
Females who are able to become pregnant:- Your healthcare provider should check to see if you are pregnant before you begin treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 6 weeks after your last dose.
- Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 3 months after your last dose.
- Tell your healthcare provider right away if your female partner becomes pregnant or thinks she may be pregnant during treatment with GOMEKLI.
-
Are breastfeeding or plan to breastfeed. It is not known if GOMEKLI passes into your breastmilk.
- Do not breastfeed during treatment with GOMEKLI and for 1 week after your last dose.
- Talk to your healthcare provider about the best way to feed your baby during this time.
How should I take GOMEKLI?
- Take GOMEKLI exactly as your healthcare provider tells you to take it. Your healthcare provider may change your dose, temporarily stop, or permanently stop treatment with GOMEKLI if you develop certain side effects.
- Take GOMEKLI twice a day, about 12 hours apart, for 21 days, followed by 7 days off treatment, to complete a 28-day treatment cycle. Your healthcare provider will decide how many treatment cycles are right for you.
- Take GOMEKLI with or without food.
- GOMEKLI comes in two different dosage forms, GOMEKLI capsules and GOMEKLI tablets for oral suspension. Your healthcare provider will decide the dosage form and dose of GOMEKLI that is right for you.
- If you take GOMEKLI capsules: Swallow each capsule whole with drinking water. If more than 1 capsule is required, swallow 1 capsule at a time. Do not open, break or chew the capsules.
-
If you take GOMEKLI tablets for oral suspension, either:
- Swallow each tablet for oral suspension whole with drinking water. If more than 1 tablet is required, swallow 1 tablet at a time. OR
- Disperse the tablets for oral suspension in drinking water to make a liquid (suspension) before you take or give GOMEKLI.
See the “Instructions for Use” that come with your medicine for instructions on how to prepare and take GOMEKLI tablets for oral suspension.
- If you miss a dose of GOMEKLI, skip the missed dose and take your next dose at your regularly scheduled time.
- If you vomit at any time after taking GOMEKLI, do not take an additional dose. Take your next dose at your regularly scheduled time.
What are the possible side effects of GOMEKLI?
GOMEKLI may cause serious side effects, including:
-
Eye problems. GOMEKLI may cause eye problems that can lead to blindness. Your healthcare provider will check your vision before and during treatment with GOMEKLI. Tell your healthcare provider right away if you get any of the following signs or symptoms of eye problems:
- Blurred vision
- Loss of vision
- Other changes to your vision
-
Heart problems. GOMEKLI may lower the amount of blood pumped by your heart, which is common in children during treatment with GOMEKLI and can also be severe. Your healthcare provider will do tests before you start GOMEKLI treatment, every 3 months during your first year of treatment, and then as needed to make sure your heart is working properly. Tell your healthcare provider right away if you get any of the following signs or symptoms of heart problems:
- Coughing or wheezing
- Shortness of breath
- Swelling of your ankles and feet
- Tiredness
- Increased heart rate
-
Skin problems. Skin rashes are common with GOMEKLI in both adults and children and can also be severe. GOMEKLI can also cause hair loss (alopecia). Tell your healthcare provider if you develop any of the following signs or symptoms of skin problems:
- Flat skin rash
- Raised bumps on the skin
- Skin bumps that look like acne
- Skin redness
- Itchy rash
- Peeling skin
The most common side effects of GOMEKLI in adults include:
- Diarrhea
- Nausea
- Muscle, joint, and bone pain
- Vomiting
- Tiredness
The most common side effects of GOMEKLI in children include:
- Diarrhea
- Muscle, joint, and bone pain
- Stomach (abdominal) pain
- Vomiting
- Headache
- Skin redness, swelling, or pain around the fingernails or toenails
- Nausea
GOMEKLI may cause fertility problems in females, which may affect your ability to have children. Talk to your healthcare provider if you have concerns about fertility.
These are not all of the possible side effects of GOMEKLI. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Please see full Prescribing Information, including Patient Information and Instructions for Use, available on GOMEKLI.com.
Text onscreen:
©2025 SpringWorks Therapeutics, Inc. All rights reserved. GOMEKLI and SpringWorks CareConnections are registered trademarks of SpringWorks Therapeutics, Inc. C_GOM_US_0412 11/25
Voice-over:
Thank you for watching.
Dispersing GOMEKLI tablets for oral suspension
View a step-by-step guide on how to prepare and then take or administer GOMEKLI as a liquid.
Petal shape from GOMEKLI logo appears onscreen, spinning as if the video is loading. Petal shape comes to a stop as full GOMEKLI logo fades in.
Image onscreen:
GOMEKLI logo shrinks and moves to top center of the frame. Indication statement appears.
Text onscreen and voice-over:
GOMEKLI (mirdametinib) is a prescription medicine used to treat adults and children 2 years of age and older with neurofibromatosis type 1 (NF1) who have plexiform neurofibromas (PN) that cause symptoms and cannot be completely removed by surgery.
It is not known if GOMEKLI is safe and effective in children under 2 years of age.
Please see Important Safety Information later in this video and Patient Information available on GOMEKLI.com.
Text onscreen:
Dispersing GOMEKLI tablets for oral suspension
Voice-over:
In this video, we’ll explain what you need to know about preparing and taking GOMEKLI as a liquid. Remember, your healthcare provider is your primary source for information on GOMEKLI.
Image onscreen:
A GOMEKLI tablet and two capsules appear onscreen. The capsules disappear, leaving only the tablet in view.
Text onscreen (under the corresponding images):
Capsules in 2 sizes
Tablets fororal suspension
Voice-over:
GOMEKLI is available in 2 forms: capsules that come in 2 sizes and tablets for oral suspension.
Image onscreen:
A GOMEKLI tablet is placed in a dosing cup filled with water. The mixture is swirled around and the liquid, now cloudy and white, settles.
Text onscreen:
Oral suspension means the tablets can mix into water.
Voice-over:
Oral suspension means the tablets mix or disperse into water, so the medicine can be taken as a liquid. This may make taking GOMEKLI easier for people who have difficulty swallowing. Follow along as we show you how to prepare GOMEKLI.
Image onscreen:
A man takes a GOMEKLI tablet with a sip of water.
Text onscreen:
GOMEKLI can be taken with or without food.
Voice-over:
The tablets can also be swallowed whole.
Image onscreen:
We see a man from behind as he reviews his GOMEKLI dosing calendar. As the voice-over plays, the sun symbols are bolded and the words “Treatment-free week” appear at the bottom of the calendar.
Text onscreen:
Take GOMEKLI by mouth twice daily for 21 days. Then, take 7 days off before resuming treatment.
Voice-over:
GOMEKLI is taken by mouth twice a day, about 12 hours apart. Each GOMEKLI dosing cycle is 28 days. You take GOMEKLI for the first 21 days, followed by a 7-day treatment break. The next cycle then begins with another 21 days of treatment.
Image onscreen:
The patient and his doctor are shown talking in the doctor’s office.
Text onscreen:
It’s important to take GOMEKLI as directed by your healthcare provider.
Voice-over:
Your healthcare provider will decide the dosage form and dose of GOMEKLI that is right for you. The following instructions are only for those who have been prescribed GOMEKLI tablets and plan to take the medicine as a liquid.
Image onscreen:
Instructions for taking GOMEKLI as a liquid are shown onscreen. As the narrator reads out each bullet point, its corresponding animated icon appears.
Text onscreen and voice-over:
Here’s what you’ll need in order to take GOMEKLI as a liquid:
- The prescribed number of GOMEKLI tablets
- A dosing cup provided by your healthcare provider or pharmacist
- About 10 to 20 milliliters of drinking water
- A 10 milliliter oral syringe, if you’re using one, provided by your healthcare provider or pharmacist
Image onscreen:
A man is shown with his supplies laid out in preparation to take GOMEKLI as a liquid.
Text onscreen:
You’re ready to GO!
Voice-over:
If you have everything that you need, it’s time to prepare GOMEKLI tablets for oral suspension.
Image onscreen:
Hands being washed in a sink and then dried.
Text onscreen:
Wash and dry your hands.
Voice-over:
Make sure your hands are clean. Wash and dry them before preparing GOMEKLI.
Image onscreen:
A dosing cup being filled with water at the sink.
Text onscreen:
Add 5 to 10 mL of water to the cup.
Voice-over:
Take the dosing cup and add 5 to 10 milliliters of drinking water to it. The amount of water doesn’t have to be exact, but be sure to only use water.
Image onscreen:
A close-up of a patient’s open hand holding two tablets.
Text onscreen:
It’s important to take GOMEKLI exactly as your doctor prescribed.
Voice-over:
Get the number of GOMEKLI tablets that your healthcare provider prescribed. Remember, it’s important to take GOMEKLI exactly as your healthcare provider told you to.
Image onscreen:
The patient drops the tablets into the dosing cup.
Text onscreen:
Add the tablets to the dosing cup.
Voice-over:
Add the prescribed number of tablets to the dosing cup.
Image onscreen:
The patient picks up the cup and swirls it around. As the tablets are dissolved into the water, it turns into a white and cloudy liquid.
Text onscreen:
Swirl the cup gently until the liquid is white and cloudy.
Voice-over:
Gently swirl the dosing cup dispersing the tablets until there aren’t any more lumps. This will take about 2 to 4 minutes. At this point, the medicine will look white and cloudy.
Image onscreen:
A hand uses a paper towel to clean up spilled GOMEKLI. Then a split screen appears: A patient washes their hands on the left side and a garbage can is shown on the right side.
Text onscreen:
Use a paper towel to clean up spilled GOMEKLI. Wash your hands afterward.
Voice-over:
Try not to spill any of the medicine during this step. If you do, use a paper towel to soak up the spilled liquid, and throw it away. Make sure to wash your hands with soap and water after throwing the paper towel away.
Image onscreen:
The patient is shown taking GOMEKLI with the dosing cup, and then the screen transitions to an image of a 30-minute timer. Finally, the shot changes to a split screen, with a timer on the left and a garbage can on the right.
Text onscreen:
Take GOMEKLI within 30 minutes of preparing it.
Voice-over:
If you’re using the dosing cup rather than a syringe to take GOMEKLI, the medicine is ready to take. Drink the GOMEKLI solution from the dosing cup right away, waiting no more than 30 minutes after preparing it. If more than 30 minutes pass, throw out the solution and start over.
Image onscreen:
The patient places the tip of the syringe into the dosing cup, the plunger is pulled back, and the liquid is transferred from the cup into the syringe.
Text onscreen:
Taking or giving GOMEKLI from an oral syringe: Draw the liquid from the dosing cup into the syringe.
Voice-over:
If you’re using an oral syringe to give the medication, place the tip of the syringe into the dosing cup, and draw up all the liquid by pulling back on the plunger.
Image onscreen:
The screen shows a close-up of a child being administered a dose of GOMEKLI with a syringe.
Text onscreen:
Place the tip of the syringe inside the mouth and slowly push the plunger down.
Voice-over:
Place the tip of the syringe inside the mouth, pointed toward the inside of either cheek. Slowly push the plunger all the way down to give the full dose of GOMEKLI and allow time for the medicine to be swallowed.
Image onscreen:
The screen shows the parent holding the syringe and the child sitting upright, waiting to receive the dose of medication.
Text onscreen:
Make sure children sit upright until they completely swallow GOMEKLI.
Voice-over:
If you’re giving GOMEKLI to a child, make sure he or she is sitting upright until all the liquid has been swallowed.
Image onscreen:
A dosing cup with residual GOMEKLI mixture is shown on the left, and a syringe with residual GOMEKLI mixture is shown on the right.
Text onscreen:
After you take the GOMEKLI mixture, there will be some left in the dosing cup.
Voice-over:
Whether you take GOMEKLI straight from the dosing cup or with the oral syringe, there will still be some medicine left in the cup afterward, even if it’s hard to see.
Image onscreen:
Person adds water to the dosing cup.
Text onscreen:
Add 5 to 10 milliliters (mL) of water to the dosing cup.
Voice-over:
To make sure that you take the entire dose, add another 5 to 10 milliliters of drinking water to the same dosing cup.
Image onscreen:
The screen splits, showing an adult patient on the left side dissolving the tablet in the dosing cup and drinking it, and a child patient on the right side having the GOMEKLI treatment administered to them with a syringe.
Text onscreen:
Follow the same steps as before to complete your dose.
Voice-over:
Gently swirl the dosing cup again and drink the mixture. If you’re using a syringe, draw the solution from the dosing cup. Place the tip of the syringe into the mouth again, and slowly push the plunger all the way down.
Image onscreen:
Person washing the dosing cup, and their hands, in a sink.
Text onscreen:
Wash and dry the dosing cup before storing it. Wash your hands when you’re done.
Voice-over:
When you’re finished, wash out the dosing cup with clean water, allowing it to dry before storing it. Wash your hands with soap when you’re done.
Image onscreen:
The screen first shows a GOMEKLI bottle placed in a cabinet with a green check mark drawn over it. Then the shot transitions into a split screen, with the first image sliding over to the left and a new image (of a GOMEKLI bottle on a windowsill in direct sunlight) appearing on the right. The image on the right has a red X placed over it, and the image on the left has a green check mark placed over it.
Text onscreen:
Store GOMEKLI at room temperature and away from light.
Voice-over:
GOMEKLI tablets should be stored at room temperature between 68 and 77 degrees Fahrenheit (or 20 and 25 degrees Celsius). Protect GOMEKLI from light.
Image onscreen:
The screen transitions to an animation of a woman’s hand holding the GOMEKLI pill bottle. The shot then widens to reveal a fuller image of the woman as she places the bottle down on the counter.
Text onscreen:
Talk to your healthcare provider or pharmacist if you have any questions.
Voice-over:
Now you know how to prepare GOMEKLI tablets for oral suspension. If you have any questions about…
Image onscreen:
Cut to a scene of a patient and his doctor in conversation at the doctor’s office.
Voice-over:
…how to prepare and take or give a dose of GOMEKLI tablets for oral suspension, talk to your healthcare provider or pharmacist. You can also rewatch this video at any time or read the GOMEKLI Instructions for Use.
Text onscreen and voice-over:
Important Safety Information
Before taking GOMEKLI, tell your healthcare provider about all of your medical conditions, including if you:
- Have eye problems
- Have heart problems
-
Are pregnant or plan to become pregnant. GOMEKLI can harm your unborn baby
Females who are able to become pregnant:- Your healthcare provider should check to see if you are pregnant before you begin treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 6 weeks after your last dose.
- Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with GOMEKLI. Males with female partners who are able to become pregnant:
- Use effective birth control (contraception) during treatment with GOMEKLI and for 3 months after your last dose.
- Tell your healthcare provider right away if your female partner becomes pregnant or thinks she may be pregnant during treatment with GOMEKLI.
-
Are breastfeeding or plan to breastfeed. It is not known if GOMEKLI passes
into your breastmilk.
- Do not breastfeed during treatment with GOMEKLI and for 1 week after your last dose.
- Talk to your healthcare provider about the best way to feed your baby during this time.
Tell your healthcare provider about all the medicines you take, including
prescription and over-the-counter medicines, vitamins, and herbal supplements.
How should I take GOMEKLI?
- Take GOMEKLI exactly as your healthcare provider tells you to take it. Your healthcare provider may change your dose, temporarily stop, or permanently stop treatment with GOMEKLI if you develop certain side effects.
- Take GOMEKLI twice a day, about 12 hours apart, for 21 days, followed by 7 days off treatment, to complete a 28-day treatment cycle. Your healthcare provider will decide how many treatment cycles are right for you.
- Take GOMEKLI with or without food.
- GOMEKLI comes in two different dosage forms, GOMEKLI capsules and GOMEKLI tablets for oral suspension. Your healthcare provider will decide the dosage form and dose of GOMEKLI that is right for you.
- If you take GOMEKLI capsules: Swallow each capsule whole with drinking water. If more than 1 capsule is required, swallow 1 capsule at a time. Do not open, break or chew the capsules.
-
If you take GOMEKLI tablets for oral suspension, either:
- Swallow each tablet for oral suspension whole with drinking water. If more than 1 tablet is required, swallow 1 tablet at a time. OR
- Disperse the tablets for oral suspension in drinking water to make a liquid (suspension) before you take or give GOMEKLI.
See the “Instructions for Use” that come with your medicine for instructions
on how to prepare and take GOMEKLI tablets for oral suspension.
- If you miss a dose of GOMEKLI, skip the missed dose and take your next dose at your regularly scheduled time.
- If you vomit at any time after taking GOMEKLI, do not take an additional dose. Take your next dose at your regularly scheduled time.
What are the possible side effects of GOMEKLI?
GOMEKLI may cause serious side effects, including:
-
Eye problems. GOMEKLI may cause eye problems that can lead to blindness.
Your healthcare provider will check your vision before and during treatment
with GOMEKLI. Tell your healthcare provider right away if you get any of the
following signs or symptoms of eye problems:
- Blurred vision
- Loss of vision
- Other changes to your vision
-
Heart problems. GOMEKLI may lower the amount of blood pumped by your heart,
which is common in children during treatment with GOMEKLI and can also be
severe. Your healthcare provider will do tests before you start GOMEKLI
treatment, every 3 months during your first year of treatment, and then as
needed to make sure your heart is working properly. Tell your healthcare
provider right away if you get any of the following signs or symptoms of
heart problems:
- Coughing or wheezing
- Shortness of breath
- Swelling of your ankles and feet
- Tiredness
- Increased heart rate
-
Skin problems. Skin rashes are common with GOMEKLI in both adults and
children and can also be severe. GOMEKLI can also cause hair loss
(alopecia). Tell your healthcare provider if you develop any of the
following signs or symptoms of skin problems:
- Flat skin rash
- Raised bumps on the skin
- Skin bumps that look like acne
- Skin redness
- Itchy rash
- Peeling skin
The most common side effects of GOMEKLI in adults include:
- Diarrhea
- Nausea
- Muscle, joint, and bone pain
- Vomiting
- Tiredness
The most common side effects of GOMEKLI in children include:
- Diarrhea
- Muscle, joint, and bone pain
- Stomach (abdominal) pain
- Vomiting
- Headache
- Skin redness, swelling, or pain around the fingernails or toenails
- Nausea
The most common severe abnormal blood tests in children include decreased white blood cell (neutrophil) counts and increased CPK.
GOMEKLI may cause fertility problems in females, which may affect your ability to have children. Talk to your healthcare provider if you have concerns about fertility.
These are not all of the possible side effects of GOMEKLI. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Please see full Prescribing Information, including Patient Information and Instructions for Use, available on GOMEKLI.com.
Text onscreen:
Thank you!
©2025 SpringWorks Therapeutics, Inc. All rights reserved. GOMEKLI is a registered trademark of SpringWorks Therapeutics, Inc. C_GOM_US_0431 8/25
Voice-over:
Thank you for watching.
Setting up your GOMEKLI dosing calendar
See how to set up your personal GOMEKLI dosing calendar so you can stay on top of treatment.
Petal shape from GOMEKLI logo appears onscreen, spinning as if the video is loading. Petal shape comes to a stop as full GOMEKLI logo fades in.
Image onscreen:
GOMEKLI logo shrinks and moves to top center of the frame. Indication statement appears.
Text onscreen and voice-over:
GOMEKLI (mirdametinib) is a prescription medicine used to treat adults and children 2 years of age and older with neurofibromatosis type 1 (NF1) who have plexiform neurofibromas (PN) that cause symptoms and cannot be completely removed by surgery.
It is not known if GOMEKLI is safe and effective in children under 2 years of age.
Please see Important Safety Information later in this video and Patient Information available on GOMEKLI.com.
Image onscreen:
Screen fades and the video title appears. Flag with the logo in the top right corner of the frame appears, where it remains for the entirety of the video.
Text onscreen:
Setting up your GOMEKLI dosing calendar
Voice-over:
Today we’re going to talk about how to set up a GOMEKLI dosing calendar for you or the person you care for to help keep track of GOMEKLI twice-daily dosing.
Image onscreen:
A calendar with a month’s worth of days. The calendar animates to show specific dates.
Text onscreen:
GOMEKLI dosing calendar
Voice-over:
Let’s quickly review the GOMEKLI dosing schedule.
Text onscreen:
Twice-daily dosing, 12 hours apart
Image onscreen:
One by one, the days of the calendar are filled in with x’s for the first 21 days of the GOMEKLI cycle.
Text onscreen:
3 weeks of treatment followed by a treatment-free week
Voice-over:
GOMEKLI is taken by mouth twice a day, about 12 hours apart. Each GOMEKLI dosing cycle is 28 days. You take GOMEKLI for the first 21 days, and then for the last 7 days of the cycle, GOMEKLI is not taken. You can think of this as 3 weeks of treatment followed by a week-long treatment break.
Image onscreen:
The calendar begins to tilt, and the x’s disappear.
Text onscreen:
After the cycle ends, start over.
Image onscreen:
A hand holding a pen enters the frame. The date is filled in for the first day on the calendar, and then the corresponding sun icon is marked with an x. The rest of the dates appear.
Voice-over:
After the treatment-free week, you start over and the next cycle begins with 21 days of GOMEKLI treatment.
Image onscreen:
The SpringWorks CareConnections® logo.
Voice-over:
Once your doctor prescribes GOMEKLI, you can enroll in our free, personalized patient support program: SpringWorks CareConnections. They’ll send you a kit that includes a pillbox and calendar, which can be used to keep track of your dosing schedule.
Image onscreen:
A bag emblazoned with the GOMEKLI logo holds a pillbox and the dosing calendar. The patient starter kit disappears, and a kitchen scene appears. A man places the dosing calendar on a refrigerator.
Voice-over:
The calendar is a small magnetic dry-erase board that you can place on your refrigerator or another magnetic surface. Be sure to place the calendar somewhere visible so you never miss a dose.
Image onscreen:
The dosing calendar with a hand filling in the dates.
Text onscreen:
Start by filling out the dates.
Voice-over:
Using the dry-erase pen that comes with the board, fill in the boxes with the dates of your dosing cycle, including the 3 weeks of treatment as well as the treatment-free week, or 28 days total.
Image onscreen:
A man stands in front of his refrigerator holding a cup in one hand and a pill in the other.
Voice-over:
Each day, cross out the sun after taking or giving the morning dose of GOMEKLI.
Image onscreen:
The screen splits. On the left is the man; on the right is the dosing calendar. He takes the dose, and the sun gets crossed out.
Text onscreen:
Sun = morning dose
Voice-over:
Each day, cross out the sun after taking or giving the morning dose of GOMEKLI.
Image onscreen:
On the left is a close-up of a clock. Its hands rotate around the dial, starting and ending at 9 o'clock. On the right, there is a window; through it, the sky turns from day to night.
Text onscreen:
Moon = nighttime dose
Voice-over:
After taking or giving the nighttime dose, go back and cross out the moon.
Image onscreen:
The window is replaced with a close-up of the calendar. The moon gets crossed off. Then, the calendar fills the whole screen, and the mornings and nights of all the days of the month are crossed off.
Voice-over:
During the treatment-free week, keep marking off the days so you know when to start the next cycle. It’s that easy!
Image onscreen:
The man stands in front of his refrigerator erasing the dates from his GOMEKLI calendar.
Voice-over:
After the calendar is all filled in, you can just erase all the markings and begin adding dates for the next cycle.
Image onscreen:
A hand holding a bottle of GOMEKLI.
Voice-over:
It’s important to stay on track with GOMEKLI treatment and take or give the medication as directed by your doctor.
Image onscreen:
A close-up of the calendar; a pen circles the sun icon. The screen splits, and the man takes his next dose of GOMEKLI.
Voice-over:
If you miss a dose of GOMEKLI, skip the missed dose and take or give the next dose at your regularly scheduled time.
Image onscreen:
The man in his bathroom brushing his teeth.
Voice-over:
There are other ways to stay on track with GOMEKLI. You can pair it with another daily routine, for example, before or after brushing your teeth in the morning and at night.
Image onscreen:
The GOMEKLI pillbox. A case comes out of the box.
Text onscreen:
The pillbox has removable containers, so you can take GOMEKLI on the go.
Voice-over:
The pillbox included in the patient starter kit can also help you keep track of each dose. It includes 7 small containers, one for each day of the week. Each container has 2 compartments labeled AM and PM for your daytime and nighttime doses.
Image onscreen:
Two capsules, one on either side of an individual pill case. The capsules move into the case's individual compartments. The case closes and moves back into the pillbox.
Text onscreen:
Keep GOMEKLI and all medicines out of the reach of children.
Voice-over:
Fill the container with the appropriate amount of GOMEKLI capsules or tablets at the start of a treatment week. When the week is over and the box is empty, you can refill it and start over.
Image onscreen:
A mobile phone with a reminder alert on the screen.
Voice-over:
You can also set up dosing reminders on your phone using the GOMEKLI Digital Companion.
Image onscreen:
A phone screen showing the option to download the Medisafe app appears. Then the icons for Medisafe, Android, and Apple appear at right.
Voice-over:
The GOMEKLI Digital Companion is a free resource for people taking GOMEKLI, available on the Medisafe medication management app.
Image onscreen:
The man downloads the app and then uses it to set up a medication reminder.
Voice-over:
After downloading the Medisafe app and creating a profile, you can set up your GOMEKLI dosing calendar and add medication reminders so you never miss a dose.
Image onscreen:
The animation zooms out. The man holds his phone as he continues to configure the app.
Text onscreen:
Be sure to inform your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Voice-over:
You can track all your medications, vitamins, and supplements with Medisafe, as well as set up refill reminders and reminders for doctor’s appointments.
Image onscreen:
A phone screen in close-up shows the support page from GOMEKLI.com.
Voice-over:
You can learn more about the GOMEKLI Digital Companion at GOMEKLI.com.
Image onscreen:
The man in his kitchen, standing at his counter drinking a cup of coffee, looks at the GOMEKLI dosing calendar.
Voice-over:
Good luck setting up your GOMEKLI dosing calendar. Feel free to rewatch this video at any time and explore additional resources at GOMEKLI.com.
Text onscreen and voice-over:
Important Safety Information
Before taking GOMEKLI, tell your healthcare provider about all of your medical conditions, including if you:
- Have eye problems
- Have heart problems
- Are pregnant or plan to become pregnant. GOMEKLI can harm your unborn baby
- Females who are able to become pregnant:
- Your healthcare provider should check to see if you are pregnant before you begin treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 6 weeks after your last dose.
- Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with GOMEKLI.
- Males with female partners who are able to become pregnant:
- Use effective birth control (contraception) during treatment with GOMEKLI and for 3 months after your last dose.
- Tell your healthcare provider right away if your female partner becomes pregnant or thinks she may be pregnant during treatment with GOMEKLI.
- Are breastfeeding or plan to breastfeed. It is not known if GOMEKLI passes into your breastmilk.
- Do not breastfeed during treatment with GOMEKLI and for 1 week after your last dose.
- Talk to your healthcare provider about the best way to feed your baby during this time.
How should I take GOMEKLI?
- Take GOMEKLI exactly as your healthcare provider tells you to take it. Your healthcare provider may change your dose, temporarily stop, or permanently stop treatment with GOMEKLI if you develop certain side effects.
- Take GOMEKLI twice a day, about 12 hours apart, for 21 days, followed by 7 days off treatment, to complete a 28-day treatment cycle. Your healthcare provider will decide how many treatment cycles are right for you.
- Take GOMEKLI with or without food.
- GOMEKLI comes in two different dosage forms, GOMEKLI capsules and GOMEKLI tablets for oral suspension. Your healthcare provider will decide the dosage form and dose of GOMEKLI that is right for you.
- If you take GOMEKLI capsules: Swallow each capsule whole with drinking water. If more than 1 capsule is required, swallow 1 capsule at a time. Do not open, break or chew the capsules.
- If you take GOMEKLI tablets for oral suspension, either:
- Swallow each tablet for oral suspension whole with drinking water. If more than 1 tablet is required, swallow 1 tablet at a time.
- OR
- Disperse the tablets for oral suspension in drinking water to make a liquid (suspension) before you take or give GOMEKLI.
- See the “Instructions for Use” that come with your medicine for instructions on how to prepare and take GOMEKLI tablets for oral suspension.
- If you miss a dose of GOMEKLI, skip the missed dose and take your next dose at your regularly scheduled time.
- If you vomit at any time after taking GOMEKLI, do not take an additional dose. Take your next dose at your regularly scheduled time.
What are the possible side effects of GOMEKLI?
GOMEKLI may cause serious side effects, including:
- Eye problems. GOMEKLI may cause eye problems that can lead to blindness. Your healthcare provider will check your vision before and during treatment with GOMEKLI. Tell your healthcare provider right away if you get any of the following signs or symptoms of eye problems:
- Blurred vision
- Loss of vision
- Other changes to your vision
- Heart problems. GOMEKLI may lower the amount of blood pumped by your heart, which is common in children during treatment with GOMEKLI and can also be severe. Your healthcare provider will do tests before you start GOMEKLI treatment, every 3 months during your first year of treatment, and then as needed to make sure your heart is working properly. Tell your healthcare provider right away if you get any of the following signs or symptoms of heart problems:
- Coughing or wheezing
- Shortness of breath
- Swelling of your ankles and feet
- Tiredness
- Increased heart rate
- Skin problems. Skin rashes are common with GOMEKLI in both adults and children and can also be severe. GOMEKLI can also cause hair loss (alopecia). Tell your healthcare provider if you develop any of the following signs or symptoms of skin problems:
- Flat skin rash
- Raised bumps on the skin
- Skin bumps that look like acne
- Skin redness
- Itchy rash
- Peeling skin
The most common side effects of GOMEKLI in adults include:
- Diarrhea
- Nausea
- Muscle, joint, and bone pain
- Vomiting
- Tiredness
The most common side effects of GOMEKLI in children include:
- Diarrhea
- Muscle, joint, and bone pain
- Stomach (abdominal) pain
- Vomiting
- Headache
- Skin redness, swelling, or pain around the fingernails or toenails
- Nausea
GOMEKLI may cause fertility problems in females, which may affect your ability to have children. Talk to your healthcare provider if you have concerns about fertility.
These are not all of the possible side effects of GOMEKLI. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Please see full Prescribing Information, including Patient Information and Instructions for Use, available on GOMEKLI.com.
Text onscreen:
Thank you!
©2025 SpringWorks Therapeutics, Inc. All rights reserved. GOMEKLI and SpringWorks CareConnections are registered trademarks of SpringWorks Therapeutics, Inc. All other trademarks and logos are the property of their respective owners. C_GOM_US_0433 8/25
Voice-over:
Thank you for watching.
Managing possible side effects of GOMEKLI
Learn how to work with your care team to manage the possible side effects of GOMEKLI.
Petal shape from GOMEKLI logo appears onscreen, spinning as if the video is loading. Petal shape comes to a stop as full GOMEKLI logo fades in.
Image onscreen:
GOMEKLI logo shrinks and moves to top center of the frame. Indication statement appears.
Text onscreen and voice-over:
GOMEKLI (mirdametinib) is a prescription medicine used to treat adults and children 2 years of age and older with neurofibromatosis type 1 (NF1) who have plexiform neurofibromas (PN) that cause symptoms and cannot be completely removed by surgery.
It is not known if GOMEKLI is safe and effective in children under 2 years of age.
Please see Important Safety Information later in this video and Patient Information available on GOMEKLI.com.
Image onscreen:
GOMEKLI logo fades and a flag with the logo in the top right corner of the frame appears, where it remains for the entirety of the video. Title of video fades in.
Text onscreen:
Managing possible side effects of GOMEKLI
Voice-over:
In this video, we’ll talk about how to work with your care team to manage common side effects and offer tips that may help throughout treatment.
Image onscreen:
Word bubbles pop up around a woman as the different side effects are introduced. The woman shrinks and moves to the bottom left of the screen as the child comes into view. The word bubble bubbles pop up around him as pediatric symptoms are introduced. The shot pans to the woman sitting across from her doctor.
Voice-over:
The most common side effects with GOMEKLI are diarrhea, nausea, muscle, joint, and bone pain, and vomiting. Some adults may also experience tiredness, while some children may experience headache, stomach pain, and skin redness, swelling, or pain around the fingernails and toenails.
GOMEKLI can cause other side effects, including some serious side effects which we will go over in this video.
Most of the side effects associated with GOMEKLI have been shown to start early in treatment, but it’s good to know that there are things your care team can do to help address them.
Image onscreen:
The camera zooms in to the woman’s arm with a rash. Different rash types appear in word bubbles around her as they are introduced.
Text onscreen:
One of the most common side effects with GOMEKLI is rash.
Voice-over:
In the single-arm clinical study of GOMEKLI, one of the most common side effects seen among both adults and children was rash, which can be severe. This could be a flat skin rash, raised bumps on the skin, skin bumps that look like acne, skin redness, itchy rash, or peeling skin.
Image onscreen:
The woman is shown with her doctor as she examines her rash. The screen splits. On the left the woman in a bathtub. On the right, the woman is applying lotion to her arm.
Text onscreen:
This information is not intended to replace the advice of your care team or other healthcare provider.
Voice-over:
There are things you can do to help address skin-related side effects. These include taking daily baths and using mild cleansers and skin moisturizers at least twice a day to prevent dryness. You may also consider avoiding products that could dry out or irritate your skin.
Image onscreen:
A doctor types up a prescription for her patient.
Text onscreen:
Tell your care team if you develop any signs or symptoms of skin problems.
Voice-over:
Your care team may also provide medication to help with the rash or refer you to a dermatologist for additional care.
Image onscreen:
A woman holds her stomach in discomfort. Different types of gastrointestinal appear in word bubbles around her as they are introduced.
Text onscreen:
Diarrhea, nausea, vomiting, and abdominal pain are also common side effects.
Voice-over:
Gastrointestinal side effects, such as diarrhea, nausea, vomiting, and abdominal pain, are also common in people who take GOMEKLI.
Image onscreen:
Food icons of french fries, hot peppers, and potato chips appear on screen in large white circles and lines going through them. They disappear and a glass appears onscreen. The shot pans to a pharmacy where the woman is looking at different medications.
Text onscreen:
This information is not intended to replace the advice of your care team or other healthcare provider.
Voice-over:
There are certain tips you can keep in mind to address stomach-related side effects, such as avoiding fried, fatty, or spicy foods, and increasing your fluid intake. If you continue to experience issues, consult your care team for further treatment options.
Image onscreen:
The woman is shown speaking with her doctor. The doctor nods and takes notes.
Text onscreen:
Take GOMEKLI as directed by your healthcare provider.
Voice-over:
Depending on what you’re experiencing, your care team may interrupt, reduce, or permanently stop your GOMEKLI treatment. It is important that you take GOMEKLI as directed by your healthcare provider.
Image onscreen:
The woman nods her head as she continues speaking with her doctor. The serious side effects pop up in word bubbles around her. The doctor then begins to examine her eyes.
Text onscreen:
GOMEKLI can cause eye and heart problems that can be serious.
Voice-over:
Because GOMEKLI can cause serious side effects, including eye problems and heart problems, your care team will regularly assess your eyes and heart before and throughout treatment. Before taking GOMEKLI, make sure to tell your healthcare provider if you have any eye or heart problems.
Image onscreen:
The doctor and woman discuss her lab results.
Text onscreen:
Your care team will conduct blood tests.
Voice-over:
Your care team will also want to run routine lab work, including blood tests. These assessments are important because they help your care team see if anything is going on that needs to be addressed.
Image onscreen:
The woman checks her phone. The camera zooms in on her screen, where it shows her scrolling through her contact list.
Text onscreen:
Regular check-ins with your care team are extremely important.
Voice-over:
That’s why it’s vital to stay on top of appointments.
Image onscreen:
The woman clicks on the contact for her care team. The screen splits: On the left the woman has the phone to her ear and on the right a doctor also has a phone to her ear.
Text onscreen:
Tell your care team immediately if you notice anything out of the ordinary.
Voice-over:
But remember, if you’re experiencing anything out of the ordinary, you shouldn’t wait until your next appointment to let your care team know. The key to staying on top of side effects is being proactive, open, and honest with your care team. They won’t know how to help you if you don’t speak up!
Image onscreen:
The GOMEKLI treatment journal appears. The pages turn so viewers can see what it looks like and how it works. We fade to the woman sitting at a desk reading through the treatment journal.
Text onscreen:
Use the treatment journal to track your appointments, how you’re feeling, and more.
Voice-over:
The GOMEKLI treatment journal can make things easier. It includes weekly templates so you can record how you’re feeling, jot down general notes, and save any questions you have for your care team. Once you start GOMEKLI and are enrolled in SpringWorks CareConnections, the journal will be sent to you as part of your GOMEKLI starter kit. You can also find it on GOMEKLI.com.
Image onscreen:
The treatment journal goes away and is replaced with a laptop. On the laptop screen is GOMEKLI.com resource page, which is being scrolled through.
Text onscreen:
Find more helpful resources on GOMEKLI.com.
Voice-over:
GOMEKLI.com also has other helpful resources in case you have questions about treatment.
Image onscreen:
The woman continues to explore GOMEKLI.com and makes her way to the SpringWorks CareConnections® page.
Text onscreen:
The SpringWorks CareConnections® Patient Support Program is not intended to take the place of your healthcare provider, and our team of Nurse Advocates cannot provide medical or clinical advice.
Voice-over:
Additionally, once you’re enrolled in SpringWorks CareConnections, our team of Nurse Advocates will be available to provide support and help you stay on track with treatment.
Image onscreen:
QUICK CUTS: Woman takes notes in her journal. She calls her doctor. Doctor is shown speaking on the phone.
Voice-over:
Managing side effects is a team effort involving both you and your care team. Keeping an open line of communication is key to ensuring you have the best experience possible with GOMEKLI. If you have any questions or concerns, please reach out to your healthcare provider. Keep watching for additional important information on side effects with GOMEKLI.
Text onscreen and voice-over:
Important Safety Information
Before taking GOMEKLI, tell your healthcare provider about all of your medical conditions, including if you:
- Have eye problems
- Have heart problems
-
Are pregnant or plan to become pregnant. GOMEKLI can harm your unborn baby
- Your healthcare provider should check to see if you are pregnant before you begin treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 6 weeks after your last dose.
- Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with GOMEKLI. Males with female partners who are able to become pregnant:
- Use effective birth control (contraception) during treatment with GOMEKLI and for 3 months after your last dose.
- Tell your healthcare provider right away if your female partner becomes pregnant or thinks she may be pregnant during treatment with GOMEKLI.
Females who are able to become pregnant: -
Are breastfeeding or plan to breastfeed. It is not known if GOMEKLI passes
into your breastmilk.
- Do not breastfeed during treatment with GOMEKLI and for 1 week after your last dose.
- Talk to your healthcare provider about the best way to feed your baby during this time.
Tell your healthcare provider about all the medicines you take, including
prescription and over-the-counter medicines, vitamins, and herbal supplements.
How should I take GOMEKLI?
- Take GOMEKLI exactly as your healthcare provider tells you to take it. Your healthcare provider may change your dose, temporarily stop, or permanently stop treatment with GOMEKLI if you develop certain side effects.
- Take GOMEKLI twice a day, about 12 hours apart, for 21 days, followed by 7 days off treatment, to complete a 28-day treatment cycle. Your healthcare provider will decide how many treatment cycles are right for you.
- Take GOMEKLI with or without food.
- GOMEKLI comes in two different dosage forms, GOMEKLI capsules and GOMEKLI tablets for oral suspension. Your healthcare provider will decide the dosage form and dose of GOMEKLI that is right for you.
- If you take GOMEKLI capsules: Swallow each capsule whole with drinking water. If more than 1 capsule is required, swallow 1 capsule at a time. Do not open, break or chew the capsules.
-
If you take GOMEKLI tablets for oral suspension, either:
- Swallow each tablet for oral suspension whole with drinking water. If more than 1 tablet is required, swallow 1 tablet at a time. OR
- Disperse the tablets for oral suspension in drinking water to make a liquid (suspension) before you take or give GOMEKLI.
See the “Instructions for Use” that come with your medicine for instructions
on how to prepare and take GOMEKLI tablets for oral suspension.
- If you miss a dose of GOMEKLI, skip the missed dose and take your next dose at your regularly scheduled time.
- If you vomit at any time after taking GOMEKLI, do not take an additional dose. Take your next dose at your regularly scheduled time.
What are the possible side effects of GOMEKLI?
GOMEKLI may cause serious side effects, including:
-
Eye problems. GOMEKLI may cause eye problems that can lead to blindness.
Your healthcare provider will check your vision before and during treatment
with GOMEKLI. Tell your healthcare provider right away if you get any of the
following signs or symptoms of eye problems:
- Blurred vision
- Loss of vision
- Other changes to your vision
-
Heart problems. GOMEKLI may lower the amount of blood pumped by your heart,
which is common in children during treatment with GOMEKLI and can also be
severe. Your healthcare provider will do tests before you start GOMEKLI
treatment, every 3 months during your first year of treatment, and then as
needed to make sure your heart is working properly. Tell your healthcare
provider right away if you get any of the following signs or symptoms of
heart problems:
- Coughing or wheezing
- Shortness of breath
- Swelling of your ankles and feet
- Tiredness
- Increased heart rate
-
Skin problems. Skin rashes are common with GOMEKLI in both adults and
children and can also be severe. GOMEKLI can also cause hair loss
(alopecia). Tell your healthcare provider if you develop any of the
following signs or symptoms of skin problems:
- Flat skin rash
- Raised bumps on the skin
- Skin bumps that look like acne
- Skin redness
- Itchy rash
- Peeling skin
The most common side effects of GOMEKLI in adults include:
- Diarrhea
- Nausea
- Muscle, joint, and bone pain
- Vomiting
- Tiredness
The most common severe abnormal blood tests in adults include an increased enzyme called creatine phosphokinase (CPK).
The most common side effects of GOMEKLI in children include:
- Diarrhea
- Muscle, joint, and bone pain
- Stomach (abdominal) pain
- Vomiting
- Headache
- Skin redness, swelling, or pain around the fingernails or toenails
- Nausea
The most common severe abnormal blood tests in children include decreased white blood cell (neutrophil) counts and increased CPK.
GOMEKLI may cause fertility problems in females, which may affect your ability to have children. Talk to your healthcare provider if you have concerns about fertility.
These are not all of the possible side effects of GOMEKLI. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Please see full Prescribing Information, including Patient Information and Instructions for Use, available on GOMEKLI.com.
Text onscreen:
Thank you!
©2025 SpringWorks Therapeutics, Inc. All rights reserved. GOMEKLI and SpringWorks Therapeutics are registered trademarks of SpringWorks Therapeutics, Inc. C_GOM_US_0432 8/25
Voice-over:
Thank you for watching.
Staying on track with treatment
Hear some tips on how to stay engaged in your care and on top of your GOMEKLI treatment over time.
Petal shape from GOMEKLI logo appears onscreen, spinning as if the video is loading. Petal shape comes to a stop as full GOMEKLI logo fades in.
Image onscreen:
GOMEKLI logo shrinks and moves to top center of the frame. Indication statement appears.
Text onscreen and voice-over:
GOMEKLI (mirdametinib) is a prescription medicine used to treat adults and children 2 years of age and older with neurofibromatosis type 1 (NF1) who have plexiform neurofibromas (PN) that cause symptoms and cannot be completely removed by surgery.
It is not known if GOMEKLI is safe and effective in children under 2 years of age.
Please see Important Safety Information later in this video and Patient Information available on GOMEKLI.com.
Image onscreen:
Screen fades and the video title appears.
Text onscreen:
Staying on track with treatment
Voice-over:
If you’ve started on GOMEKLI, congratulations! You’ve taken the first step of your new journey.
Image onscreen:
A man taking a GOMEKLI bottle from his medicine cabinet and taking his dose.
Voice-over:
The next step—and this is really important—is staying on track with your treatment. In this video, we’ll share some tips on how to stay engaged in your care and on top of your GOMEKLI treatment over time.
Image onscreen:
A man examining his arm.
Voice-over:
Once you start taking GOMEKLI, it may take some time to know if you’re responding to treatment. While you may not see immediate results, don’t get discouraged—keep taking your medication as prescribed.
Image onscreen:
A calendar, a pillbox, and a cellphone coming out of a tote bag.
Voice-over:
Everyone tracks their treatment progress in different ways, which is why we’ve designed various tools to suit your needs.
Image onscreen:
The SpringWorks CareConnections logo.
Text onscreen:
SpringWorks CareConnections®: a free, personalized patient support program
Voice-over:
Once you start GOMEKLI and enroll in the SpringWorks CareConnections support program, you’ll be sent a GOMEKLI starter kit.
Image onscreen:
The GOMEKLI dosing calendar appears with dates filling in.
Voice-over:
The GOMEKLI starter kit includes a dosing calendar that you can use to keep track of each dose. It’s a small dry-erase board you can hang right on your refrigerator and reuse for each treatment cycle.
Image onscreen:
A woman affixing the calendar to her refrigerator, and her son marks an “x” on one of the dates.
Voice-over:
If you’re caring for a child or adolescent who’s taking GOMEKLI, have them fill out the calendar along with you. Using it together to track their doses is a nice way for you to help them become more engaged and proactive in their treatment.
Image onscreen:
The weekly pillbox showing one of the daily containers with AM and PM icons on top.
Voice-over:
Also included in the GOMEKLI starter kit is a weekly pillbox. The pillbox includes daily containers that are split into AM and PM compartments to hold your morning and nighttime doses. This can be a helpful resource, whether you’re home or on the go, so you don’t forget to take your medication.
Image onscreen:
A finger tapping on a phone screen to download the Medisafe medication management app.
Voice-over:
Another available tool is the GOMEKLI Digital Companion. It’s a free resource for people taking GOMEKLI, available on the Medisafe medication management app. After downloading the Medisafe app and creating a profile, you can set up your GOMEKLI dosing calendar and add medication reminders, so you never miss a dose. You can learn more about the GOMEKLI dosing calendar, pillbox, and Digital Companion in the “Setting up your GOMEKLI dosing calendar” video on GOMEKLI.com.
Image onscreen:
A doctor’s exam room where a man and his doctor are talking.
Voice-over:
Taking GOMEKLI as prescribed by your healthcare provider is critical. It’s also important to stay vigilant with your appointments because even if you’re not experiencing symptoms, regular appointments are the best way for your healthcare provider to properly assess your progress and make sure things are going well.
Image onscreen:
The personalized treatment journal appears.
Voice-over:
The personalized treatment journal can be used to keep notes on how you’re feeling so your care team knows how you’re doing on GOMEKLI. The treatment journal is included in the GOMEKLI starter kit and can also be downloaded on GOMEKLI.com.
Image onscreen:
A man sitting on his couch reviewing his personalized treatment journal.
Voice-over:
If you change healthcare providers, you can always refer back to your journal as a record of your treatment history. Additionally, once you’re enrolled in SpringWorks CareConnections, you’ll have access to one-on-one support from our team of Nurse Advocates.
Image onscreen:
A man sitting at his computer about to click the “Enroll now” button.
Text onscreen:
The SpringWorks CareConnections® Patient Support Program is not intended to take the place of your healthcare provider, and our team of Nurse Advocates cannot provide medical or clinical advice.
Voice-over:
Nurse Advocates serve as a dedicated single point of contact at SpringWorks CareConnections for patients throughout their GOMEKLI treatment.
Image onscreen:
A Nurse Advocate speaking with a man over the phone.
Voice-over:
They can help you stay on track and take your medication, help you plan conversations with your care team, and work with your healthcare provider and pharmacy so you receive GOMEKLI as prescribed, including prescription refill reminders. And don’t forget, the GOMEKLI patient website has a library of resources designed to support you throughout your GOMEKLI treatment.
Image onscreen:
The man grabs his belongings and walks out of the house.
Voice-over:
Remember, NF1-PN is a long-term condition that may require long-term treatment. Staying on track with your care and treatment will give you the best chance of seeing results.
Text onscreen and voice-over:
Important Safety Information
Before taking GOMEKLI, tell your healthcare provider about all of your medical conditions, including if you:
- Have eye problems
- Have heart problems
-
Are pregnant or plan to become pregnant. GOMEKLI can harm your unborn baby
Females who are able to become pregnant:- Your healthcare provider should check to see if you are pregnant before you begin treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 6 weeks after your last dose.
- Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 3 months after your last dose.
- Tell your healthcare provider right away if your female partner becomes pregnant or thinks she may be pregnant during treatment with GOMEKLI.
-
Are breastfeeding or plan to breastfeed. It is not known if GOMEKLI passes into your breastmilk.
- Do not breastfeed during treatment with GOMEKLI and for 1 week after your last dose.
- Talk to your healthcare provider about the best way to feed your baby during this time.
How should I take GOMEKLI?
- Take GOMEKLI exactly as your healthcare provider tells you to take it. Your healthcare provider may change your dose, temporarily stop, or permanently stop treatment with GOMEKLI if you develop certain side effects.
- Take GOMEKLI twice a day, about 12 hours apart, for 21 days, followed by 7 days off treatment, to complete a 28-day treatment cycle. Your healthcare provider will decide how many treatment cycles are right for you.
- Take GOMEKLI with or without food.
- GOMEKLI comes in two different dosage forms, GOMEKLI capsules and GOMEKLI tablets for oral suspension. Your healthcare provider will decide the dosage form and dose of GOMEKLI that is right for you.
- If you take GOMEKLI capsules: Swallow each capsule whole with drinking water. If more than 1 capsule is required, swallow 1 capsule at a time. Do not open, break or chew the capsules.
-
If you take GOMEKLI tablets for oral suspension, either:
- Swallow each tablet for oral suspension whole with drinking water. If more than 1 tablet is required, swallow 1 tablet at a time. OR
- Disperse the tablets for oral suspension in drinking water to make a liquid (suspension) before you take or give GOMEKLI.
See the “Instructions for Use” that come with your medicine for instructions on how to prepare and take GOMEKLI tablets for oral suspension.
- If you miss a dose of GOMEKLI, skip the missed dose and take your next dose at your regularly scheduled time.
- If you vomit at any time after taking GOMEKLI, do not take an additional dose. Take your next dose at your regularly scheduled time.
What are the possible side effects of GOMEKLI?
GOMEKLI may cause serious side effects, including:
-
Eye problems. GOMEKLI may cause eye problems that can lead to blindness. Your healthcare provider will check your vision before and during treatment with GOMEKLI. Tell your healthcare provider right away if you get any of the following signs or symptoms of eye problems:
- Blurred vision
- Loss of vision
- Other changes to your vision
-
Heart problems. GOMEKLI may lower the amount of blood pumped by your heart, which is common in children during treatment with GOMEKLI and can also be severe. Your healthcare provider will do tests before you start GOMEKLI treatment, every 3 months during your first year of treatment, and then as needed to make sure your heart is working properly. Tell your healthcare provider right away if you get any of the following signs or symptoms of heart problems:
- Coughing or wheezing
- Shortness of breath
- Swelling of your ankles and feet
- Tiredness
- Increased heart rate
-
Skin problems. Skin rashes are common with GOMEKLI in both adults and children and can also be severe. GOMEKLI can also cause hair loss (alopecia). Tell your healthcare provider if you develop any of the following signs or symptoms of skin problems:
- Flat skin rash
- Raised bumps on the skin
- Skin bumps that look like acne
- Skin redness
- Itchy rash
- Peeling skin
The most common side effects of GOMEKLI in adults include:
- Diarrhea
- Nausea
- Muscle, joint, and bone pain
- Vomiting
- Tiredness
The most common side effects of GOMEKLI in children include:
- Diarrhea
- Muscle, joint, and bone pain
- Stomach (abdominal) pain
- Vomiting
- Headache
- Skin redness, swelling, or pain around the fingernails or toenails
- Nausea
GOMEKLI may cause fertility problems in females, which may affect your ability to have children. Talk to your healthcare provider if you have concerns about fertility.
These are not all of the possible side effects of GOMEKLI. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Please see full Prescribing Information, including Patient Information and Instructions for Use, available on GOMEKLI.com.
Text onscreen:
©2025 SpringWorks Therapeutics, Inc. All rights reserved. GOMEKLI and SpringWorks CareConnections are registered trademarks of SpringWorks Therapeutics, Inc. All other trademarks and logos are the property of their respective owners. C_GOM_US_0393 11/25
Voice-over:
Thank you for watching. And remember: You’ve got this!

Talking to your doctor about GOMEKLI

Tests you may need as you get going

Support with SpringWorks CareConnections®
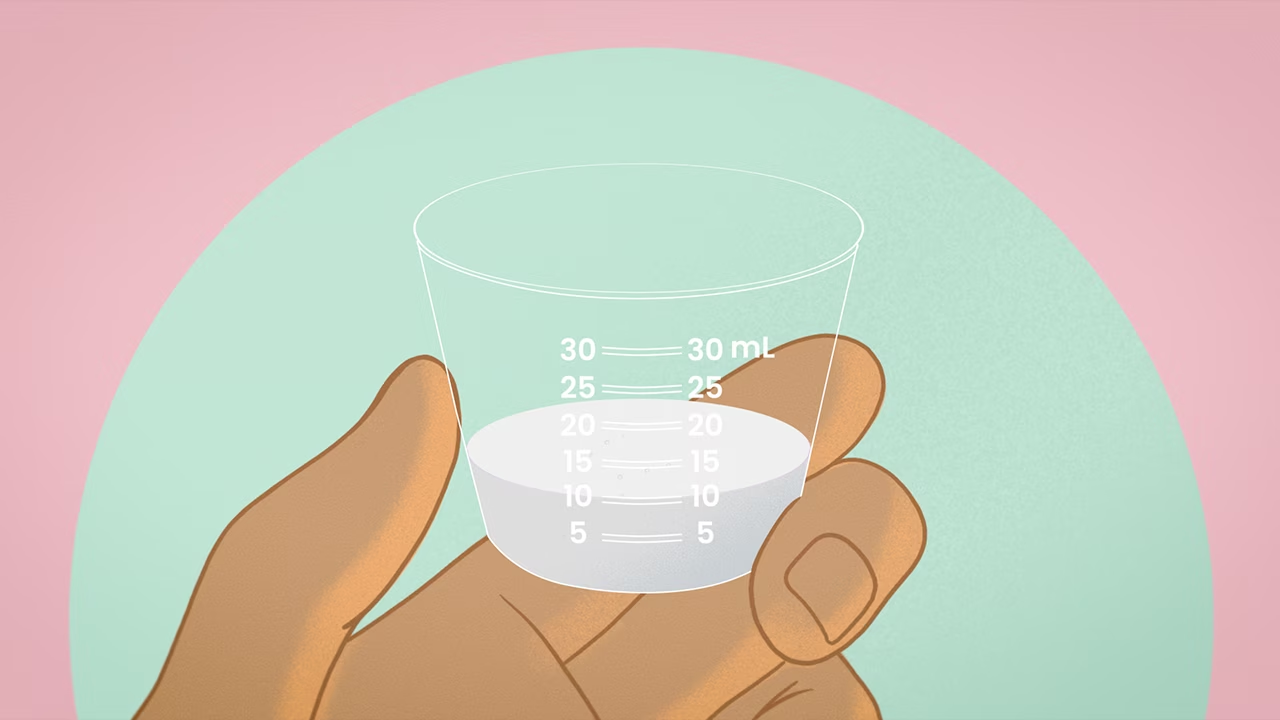
Dispersing GOMEKLI tablets for oral suspension
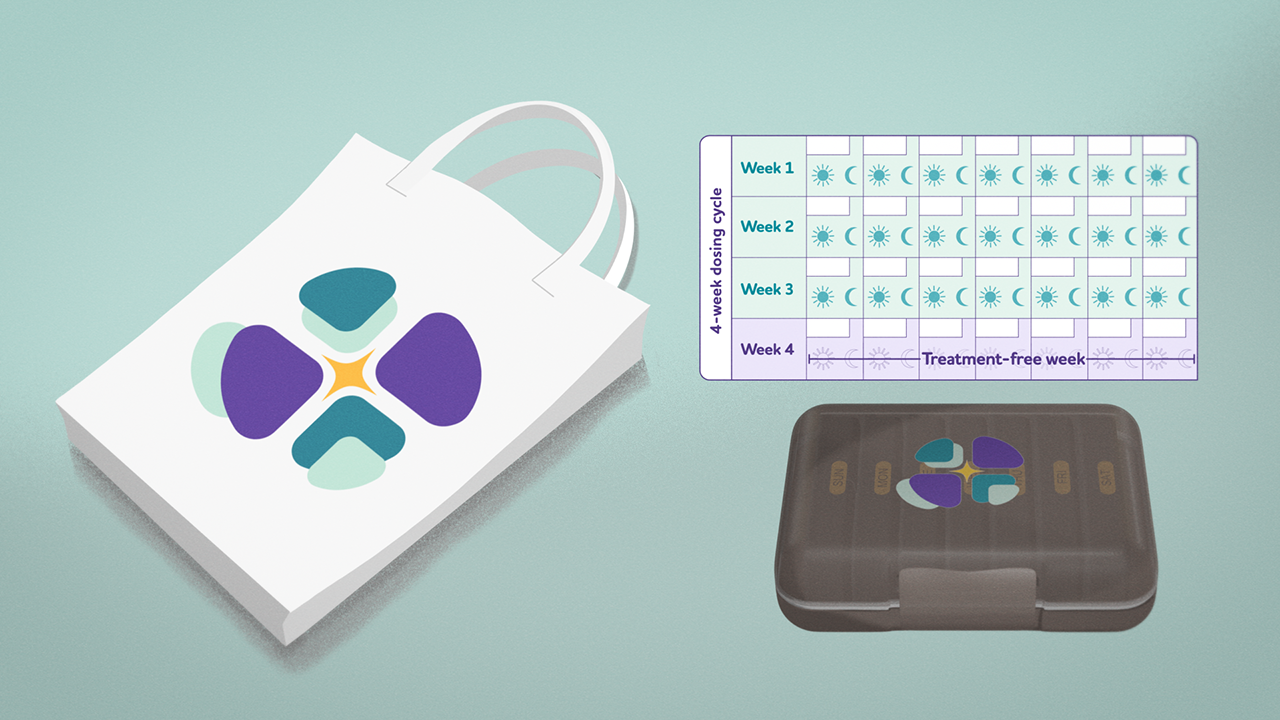
Setting up your GOMEKLI dosing calendar

Managing possible side effects of GOMEKLI

Staying on track with treatment
Meet Austin
Hear Austin talk about NF1-PN and his experience on GOMEKLI.
The video title and GOMEKLI indication statement appear onscreen with the GOMEKLI logo small in the lower right corner.
Text onscreen:
Meet Austin:
GOMEKLI Guide Patient Ambassador
Text onscreen and voice-over:
What is GOMEKLI?
GOMEKLI (mirdametinib) is a prescription medicine used to treat adults and children 2 years of age and older with neurofibromatosis type 1 (NF1) who have plexiform neurofibromas (PN) that cause symptoms and cannot be completely removed by surgery.
It is not known if GOMEKLI is safe and effective in children under 2 years of age.
Image onscreen:
We follow Austin from behind as he walks into a church, past stained-glass windows, and then down a flight of stairs. We then see him seated at a conference table in a smaller room, looking at a bible, and writing notes in his notebook.
[Austin]
Ministry for me is about showing up for people in their hardest moments. I am there as the shepherd, I’m there to remind them and guide them through those hard times. I’ve been there, I’ve done that, so I know what it means to carry something heavy, invisible, and lifelong. I’ve lived with neurofibromatosis type 1 with plexiform neurofibromas, NF1-PN, for almost my entire life. NF1 is a genetic disorder that causes non-cancerous tumors to grow along the nerves throughout the body.
Image onscreen:
Austin is seated in an interview chair, talking to at an interviewer off-camera. The background shows a living space with plants, a bookshelf, coffee table, artwork, rug, French doors, and a window. A name super graphic appears onscreen.
Text onscreen:
Austin
Living with NF1-PN and taking GOMEKLI® (mirdametinib)
Austin is being compensated by SpringWorks Therapeutics, Inc.
[Austin]
I was two and a half years old when my parents noticed a dark discoloration on my back that looked like a bruise. When it didn't go away, they took me to the doctor. Eventually, scans revealed it was a type of tumor called plexiform neurofibroma and I was diagnosed with NF1-PN. That was the beginning of this journey.
Image onscreen:
Austin is seated at a conference table in a small room. He reads a bible and makes notes in his notebook. There is a mug of tea on the table. In the background are stained-glass windows, a lamp, and a couch. Closeup shots of Austin’s hand holding a pen and writing.
[Austin]
NF1 runs in my family. My dad and grandmother both have it. But no one in the family has tumors like me. By the time I was four, I had to have surgery to remove part of it.
Image onscreen:
Austin is seated in an interview chair, talking to at an interviewer off-camera.
[Austin]
Later that year, I needed another surgery to remove more of that tumor because it was pressing back into my spine. We named my tumor Ralph the Runaway Mouse after one of my favorite children books. It helped us talk about it and normalize it. He’s just a part of me, so to speak.
Image onscreen:
Austin walks along some church pews. He is then shown seated, looking up towards the front of the church, then down at the floor. The video cuts back to the interview shot before showing Austin in the church again.
[Austin]
I was already learning that this condition was not going to be easy to live with. I remember being scared about a few things, but my parents were always honest with me about what was going on. Sometimes doctors would try to pull my parents out of the room, but my parents would tell them that “Austin has to live with this, so he needs to be involved in the conversation.” It helped me be somebody that speaks up and advocates for myself.
Image onscreen:
Austin stands in front of a large table in a room in his house. On the table there are a variety of items associated with camping, such as a lantern, first aid kit, backpack, tarp, tent, etc. He checks over the various items. He then consults a map, planning his hiking route. He packs the items in his backpack, puts on his backpack, grabs some other gear, and then exits his house through the front door. The video occasionally cuts back and forth with the interview shot.
[Austin]
Growing up, NF1-PN affected almost everything in my life. I could not always keep up physically with kids my age, so there was a lot of misunderstanding with coaches and teachers. I remember one time, at a basketball game that I got hit hard right in my tumor. And getting yelled at to get right back up when I was in excruciating pain. People don’t always see what you are carrying. When I got a little older, I started talking to doctors myself. I would tell them where it hurt, and what activities would make it worse. My NF1 specialist, treated me like a person, not just another patient. He understood that I know my own body better than anyone and pushed me to find a treatment that worked for me. We tried several pain regulation treatments to try to manage the symptoms that my plexiforms caused. There were a few years in my early twenties when I was not on treatment. My pain was manageable; I just needed a break from all the appointments. But eventually the pain came back. I was having spasms, and the pain was so intense at times, I could hardly move around. I decided to reengage with care and started seeing a new doctor.
Image onscreen:
Austin carries his backpack and gear outside towards the back of his SUV. The rear lift gate opens automatically, and Austin puts his gear in the trunk. As the trunk closes, the GOMEKLI indication statement appears along the bottom of the screen.
[Austin]
That’s when I heard about a clinical trial for a treatment called mirdametinib, what is now GOMEKLI.
Text onscreen:
GOMEKLI (mirdametinib) is a prescription medicine used to treat adults and children 2 years of age and older with neurofibromatosis type 1 (NF1) who have plexiform neurofibromas that cause symptoms and cannot be completely removed by surgery. It is not known if GOMEKLI is safe and effective in children under 2 years of age.
Image onscreen:
Austin is seated in an interview chair, talking to at an interviewer off-camera. The video then cuts to Austin standing in the forest as he consults his map and compass.
[Austin]
My doctor told me the treatment goal of GOMEKLI was to reduce the size of my plexiform tumors by at least 20%.
Image onscreen:
Austin is seated in an interview chair, talking to at an interviewer off-camera. A disclaimer graphic appears along the bottom of the screen. The video then cuts to a shot following Austin as he hikes along a trail in the forest.
Text onscreen:
Please see Important Safety Information throughout and Full Prescribing Information including Patient Information.
[Austin]
When I heard that, I was just astonished. I was in. I was excited about the idea of my tumor shrinking and hoped that it would relieve some of the symptoms I had because of my tumor.
Image onscreen:
Austin is seated in an interview chair, talking to at an interviewer off-camera. A disclaimer graphic appears along the bottom of the screen.
Text onscreen:
The most common side effects of GOMEKLI in adults include: diarrhea, nausea, muscle, joint, and bone pain, vomiting, tiredness. These are not all of the possible side effects of GOMEKLI. Call your doctor for medical advice about side effects.
[Austin]
Starting GOMEKLI was a commitment. 21 days on, 7 days off, with regular MRIs, and side effects such as rashes and digestive issues, but I worked closely with my doctor to manage these. I learned what worked for me such as staying hydrated and using baby lotion on the rash.
Image onscreen:
We see Austin from the front and side as he hikes along a path in the forest. He uses hiking poles to help with stability.
Text onscreen:
Individual results may vary.
[Austin]
And then, after a year on GOMEKLI, we got the results. A 57% reduction in the size of my tumor.
Image onscreen:
Austin is seated in an interview chair, talking to at an interviewer off-camera. The video then cuts to a wide profile shot of Austin hiking through some long grass, with a forest visible in the background.
[Austin]
I was speechless. It was the first time that something has made a noticeable difference in my NF1-PN. Those results really motivated me to stay on GOMEKLI. This is just my experience, and everyone’s experience may be different.
Image onscreen:
We see Austin in a closeup shot as he drinks water from a reusable water bottle. He then walks into his campsite and sets down a bag on a folding chair. His tent is visible in the background, which is set out on some grass surrounded by trees and bushes. There is a small folding table in front of his chair, as well as a metal firepit stocked with firewood. Austin sets up a portable gas stove and pours water into a pot, which he then puts on the stove to boil. He checks on the water and then sits in his chair, waiting for the water to boil. The video then briefly cuts back to the interview shot.
[Austin]
Now, GOMEKLI is just part of my daily routine. I take it once in the morning and once at night. It doesn’t interfere with my work or the way I want to live my life. If there’s something I could say to someone who is newly diagnosed with NF1-PN, find a doctor who listens to you. Speak up, even if you’re not sure that it matters. And you’re not alone. Reach out to others that are living with NF1-PN. Theres a whole community of us out here that understands.
Image onscreen:
Austin stands at a pulpit in a church and addresses his congregation. Behind Austin, we see lots of dark wood paneling, as well as the wall-mounted silver pipes of an organ. Stained glass windows line the sides of the room. Some shots show the backs of heads and shoulders of people as they listen to Austin preach. The video then fades to white.
[Austin]
Ministry is about being real with people. I show up not in spite of my NF1-PN, but because of it. I know pain, I know frustration. On treatment with GOMEKLI, my tumor is smaller. I have the strength and confidence to focus on the things I love.
Image onscreen:
A disclaimer with the title “Important Safety Information” fades onscreen with the GOMEKLI logo small in the lower right corner. The title and GOMEKLI logo stay in place as the text on screen changes as the presentation of Important Safety Information progresses.
Text onscreen and voice-over:
Important Safety Information
Before taking GOMEKLI, tell your healthcare provider about all of your medical conditions, including if you:
- Have eye problems
- Have heart problems
- Are pregnant or plan to become pregnant. GOMEKLI can harm your unborn baby
Females who are able to become pregnant:- Your healthcare provider should check to see if you are pregnant before you begin treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 6 weeks after your last dose.
- Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 3 months after your last dose.
- Talk to your healthcare provider about the best way to feed your baby during this time.
- Are breastfeeding or plan to breastfeed. It is not known if GOMEKLI passes
into your breastmilk.
- Do not breastfeed during treatment with GOMEKLI and for 1 week after your last dose.
- Talk to your healthcare provider about the best way to feed your baby during this time.
How should I take GOMEKLI?
- Take GOMEKLI exactly as your healthcare provider tells you to take it. Your healthcare provider may change your dose, temporarily stop, or permanently stop treatment with GOMEKLI if you develop certain side effects.
- Take GOMEKLI twice a day, about 12 hours apart, for 21 days, followed by 7 days off treatment, to complete a 28-day treatment cycle. Your healthcare provider will decide how many treatment cycles are right for you.
- Take GOMEKLI with or without food.
- GOMEKLI comes in two different dosage forms, GOMEKLI capsules and GOMEKLI tablets for oral suspension. Your healthcare provider will decide the dosage form and dose of GOMEKLI that is right for you.
- If you take GOMEKLI capsules: Swallow each capsule whole with drinking water. If more than 1 capsule is required, swallow 1 capsule at a time. Do not open, break or chew the capsules.
- If you take GOMEKLI tablets for oral suspension, either:
- Swallow each tablet for oral suspension whole with drinking water. If more than 1 tablet is required, swallow 1 tablet at a time.
- Disperse the tablets for oral suspension in drinking water to make a liquid (suspension) before you take or give GOMEKLI. See the “Instructions for Use” that come with your medicine for instructions on how to prepare and take GOMEKLI tablets for oral suspension.
- If you miss a dose of GOMEKLI, skip the missed dose and take your next dose at your regularly scheduled time.
- If you vomit at any time after taking GOMEKLI, do not take an additional dose. Take your next dose at your regularly scheduled time.
What are the possible side effects of GOMEKLI?
GOMEKLI may cause serious side effects, including:
- Eye problems. GOMEKLI may cause eye problems that can lead to blindness.
Your healthcare provider will check your vision before and during treatment
with GOMEKLI. Tell your healthcare provider right away if you get any of the
following signs or symptoms of eye problems:
- Blurred vision
- Loss of vision
- Other changes to your vision
- Heart problems. GOMEKLI may lower the amount of blood pumped by your heart,
which is common in children during treatment with GOMEKLI and can also be
severe. Your healthcare provider will do tests before you start GOMEKLI
treatment, every 3 months during your first year of treatment, and then as
needed to make sure your heart is working properly. Tell your healthcare
provider right away if you get any of the following signs or symptoms of
heart problems:
- Coughing or wheezing
- Shortness of breath
- Swelling of your ankles and feet
- Tiredness
- Increased heart rate
- Skin problems. Skin rashes are common with GOMEKLI in both adults and
children and can also be severe. GOMEKLI can also cause hair loss
(alopecia). Tell your healthcare provider if you develop any of the
following signs or symptoms of skin problems:
- Flat skin rash
- Raised bumps on the skin
- Skin bumps that look like acne
- Skin redness
- Itchy rash
- Peeling skin
- Diarrhea
- Nausea
- Muscle, joint, and bone pain
- Vomiting
- Tiredness
The most common side effects of GOMEKLI in children include:
- Diarrhea
- Muscle, joint, and bone pain
- Stomach (abdominal) pain
- Vomiting
- Headache
- Skin redness, swelling, or pain around the fingernails or toenails
- Nausea
GOMEKLI may cause fertility problems in females, which may affect your ability to have children. Talk to your healthcare provider if you have concerns about fertility.
These are not all of the possible side effects of GOMEKLI. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Please see full Prescribing Information, including Patient Information and Instructions for Use.
Image onscreen:
The GOMEKLI logo appears large in the center of the screen with disclaimer information in a single line along the bottom.
Text onscreen:
©2025 SpringWorks Therapeutics, Inc. All rights reserved. GOMEKLI is a registered trademark of SpringWorks Therapeutics, Inc. C_GOM_US_0332 07/25
Meet Julie and Jacoby
We see Jacoby sitting casually on a carpeted floor, leaning back against an armchair as he strums an electric guitar that is plugged into an amplifier. He is in a living area of a home with two armchairs, a table with a frame and houseplant, and artwork on the walls. Closeup shot of Jacoby’s left hand playing chords on the neck of the guitar.
Julie:
Jacoby has always been this bright, happy kid full of energy, full of curiosity. He loves music, sports, and just being a kid.
Image onscreen:
Julie is seated in an interview chair, talking to an interviewer off-camera. The background shows a living space with an armchair, a window seat with pillows, a piano, and a side table with stacked books. A name super graphic appears onscreen.
Text onscreen:
Julie
Mother and caregiver to Jacoby living with NF1-PN and taking GOMEKLI (mirdametinib) Julie is being compensated by SpringWorks Therapeutics, Inc.
Julie:
But behind all of that, there’s this part of his story that has shaped so much of our lives – his journey with neurofibromatosis type 1 with plexiform neurofibromas or NF1-PN.
Image onscreen:
Jacoby makes an adjustment on his amplifier by turning a couple knobs. He then continues to strum his guitar. Closeup shots of his hands and face as he plays.
Julie:
His dad and I first noticed something when Jacoby was just a few months old. He had this cute coffee colored mark on his belly. At first, we didn’t think much of it and thought it might just be a birthmark, but as we started paying more attention, we noticed more of them.
Image onscreen:
Julie is seated in an interview chair, talking to at an interviewer off-camera.
Julie:
We didn’t know what they meant. I did what most new parents would do – I searched the internet. I read that Jacoby’s marks might be something called café-au-lait spots.
Image onscreen:
We see a shot of a blue-colored lava lamp, with bubbles slowly morphing inside the lamp. The video then switches back to Jacoby as he makes some adjustments on the tuning knobs on the head of his guitar. He continues to strum the guitar, then gets up, sets his guitar down on a stand, and unplugs a cable from the amplifier.
Julie:
And that’s the first time I came across neurofibromatosis type 1, or NF1. I remember reading NF1 is a genetic disorder that can cause non-cancerous tumors to grow along nerves throughout the body.
Image onscreen:
Julie is seated in an interview chair, talking to at an interviewer off-camera.
Julie:
My heart sank. No one in our family had ever faced something like this. It wasn’t something that had ever been on our radar. But my gut told me something was wrong, and I pushed for answers.
Image onscreen:
Julie is seated on a large corner couch. The wall behind has wood wainscoting and there is a round coffee table with a tray and candle in front of Julie. She holds a photo album in her lap. Jacoby walks into frame and joins her on the couch. Together, they look through the photo album and point and reminisce over family photos.
Julie:
I brought it up to our pediatrician, but she wasn’t familiar with NF1 and initially wasn’t too concerned. She did some research, made some calls, and got us connected with the NF1 clinic at the local university. The clinic took a sample of Jacoby’s blood to run tests. When the results came back, we got the official diagnosis of NF1.
Image onscreen:
Julie is seated in an interview chair, talking to at an interviewer off-camera.
Julie:
We were scared. We didn’t know what to do. The NF1 team told us all we could do was wait and see how Jacoby’s symptoms progressed.
Image onscreen:
Julie and Jacoby continue to look through the photo album.
Julie:
For a while life felt normal. Jacoby was happy, active, hitting all of his milestones. But then, around five-years-old, he started waking up in the middle of the night with intense ankle pain. Doctors told us NF1 patients often experience pain like this, and they didn’t think it was a tumor. And then one day I pressed on his abdomen, and he jolted in pain.
Image onscreen:
Julie is seated in an interview chair, talking to at an interviewer off-camera.
Julie:
I knew something was wrong. I didn’t want my son to keep experiencing this pain and discomfort. That's when I demanded imaging.
Image onscreen:
Julie and Jacoby continue to look through the photo album.
Julie:
Jacoby’s scan showed a large plexiform neurofibroma, or PN, that could not completely be removed by surgery. It had been growing all along pressing on nerves in his abdomen and groin.
Image onscreen:
Julie is seated in an interview chair, talking to at an interviewer off-camera.
Julie:
That’s when we realized that we weren’t just dealing with NF1. We were dealing with NF1-PN. Jacoby’s tumor could keep growing, causing pain, affecting his mobility. It was terrifying.
Image onscreen:
Jacoby is seated on a bench in an ice-hockey arena. He is talking to his father, who is seated on the bench next to him. We see hockey equipment on the bench next to Jacoby. Jacoby then puts on his ice skates. Closeup shot of Jacoby tying his skate laces. A disclaimer graphic appears along the bottom of the screen.
Julie:
But our NF doctor was incredible. The moment he showed us the scan he said, “There’s a clinical trial and I think Jacoby would be perfect for it.” That’s how we first heard about mirdametinib, what is now GOMEKLI.
Text onscreen:
GOMEKLI (mirdametinib) is a prescription medicine used to treat adults and children 2 years of age and older with neurofibromatosis type 1 (NF1) who have plexiform neurofibromas that cause symptoms and cannot be completely removed by surgery. It is not known if GOMEKLI is safe and effective in children under 2 years of age.
Image onscreen:
Julie is seated in an interview chair, talking to at an interviewer off-camera.
Julie:
We talked with Jacoby’s doctor about what to expect during the trial.
Image onscreen:
Closeup shot of Jacoby grabbing his gloves off the bench. We then see Jacoby putting on his helmet and mask. He then grabs his hockey stick.
Julie:
His doctor said the treatment goal was to reduce the size of his plexiform neurofibroma by at least 20%. We trusted our doctor and wanted to do whatever we could to help Jacoby.
Image onscreen:
Julie is seated in an interview chair, talking to at an interviewer off-camera.
Julie:
We decided we wanted to be in this trial.
Image onscreen:
Jacoby and his father stand up from the bench and walk along the edge of the rink. A disclaimer graphic appears along the bottom of the screen.
Text onscreen:
Please see Important Safety Information throughout and Full Prescribing Information including Patient Information.
Julie:
We hoped with the reduction of the tumor that Jacoby might get some relief from the pressure the tumor size was causing.
Image onscreen:
Julie is seated in an interview chair, talking to at an interviewer off-camera.
Julie:
Within weeks, we noticed his symptoms had started to ease.
Image onscreen:
The camera follows Jacoby as he skates across the ice rink with his hockey stick. We see his father just outside the rink, leaning forward with his forearms resting on the divider. He watches Jacoby skate by and shouts encouragement. A disclaimer graphic appears along the bottom of the screen, followed by a second disclaimer graphic.
Text onscreen:
GOMEKLI may cause serious side effects, including: eye problems, heart problems, and skin problems. Tell your healthcare provider if you are pregnant or plan to become pregnant. GOMEKLI can harm your unborn baby.
Text onscreen:
The most common side effects of GOMEKLI in children include:
diarrhea, muscle, joint, and bone pain, stomach (abdominal) pain, vomiting, headache, skin redness, swelling, or pain around the fingernails or toenails, nausea
Julie:
Throughout treatment, he experienced some skin problems including mild rashes and skin infection, but using a cream that his doctor recommended helped. He also had nausea, vomiting, diarrhea, tumor pain, intermittent headaches, and intermittent joint pain.
Image onscreen:
Julie is seated in an interview chair, talking to at an interviewer off-camera. A disclaimer graphic appears along the bottom of the screen.
Text onscreen:
These are not all of the possible side effects of GOMEKLI. Call your doctor for medical advice about side effects.
Julie:
The off weeks when he didn’t take the medication were difficult, but we worked with his health care provider to manage the side effects through hydration, rest, and over-the-counter pain relievers.
Image onscreen:
Jacoby does a slalom exercise by skating through a line of orange cones on the ice. The video briefly cuts back to Julie’s interview shot before showing Jacoby’s father using his foot to push pucks across the ice to Jacoby. Jacoby lines up in front of the goal and uses his stick to hit the pucks from his father into the goal. A disclaimer graphic appears along the bottom of the screen.
Text onscreen:
Individual results may vary.
Julie:
He also experienced a decrease in the amount of blood pumped by his heart. This did not cause symptoms and resolved without changing the dose of GOMEKLI. But Jacoby is tough, and he stuck with it. After one year of being on GOMEKLI, we got the results we wanted, met the goals of the trial, and his tumor had shrunk. Jacoby continued on GOMEKLI as part of the optional long-term follow-up phase of the trial. As part of that, he continues to get regular MRIs.
Image onscreen:
Julie is seated in an interview chair, talking to at an interviewer off-camera.
Julie:
Jacoby was only seven years old when he started treatment with GOMEKLI and there has been partial regrowth of the PN as he has continued in the study.
Image onscreen:
Jacoby and his father have left the ice and now sit down together on a bench. Jacoby takes off his helmet and talks with his father. The video briefly cuts to Julie’s interview shot before going back to Jacoby and his father sitting on the bench. Jacoby’s father affectionately ruffles Jacoby’s hair.
Julie:
His doctor has told us that this happens in some patients, and he remains on GOMEKLI treatment. I still believe that starting GOMEKLI and continuing on GOMEKLI is the right choice for us. This is just our experience and every patient’s experience is different.
Image onscreen:
Jacoby is seated in an interview chair, talking to at an interviewer off-camera. The background shows a living area with chairs, French doors leading to another room, and artwork on the walls. A name super graphic appears onscreen.
Text onscreen:
Jacoby
Living with NF1-PN and taking GOMEKLI (mirdametinib)
Jacoby is being compensated by SpringWorks Therapeutics, Inc.
Jacoby:
When I go in to talk to my doctor, he’s really down to earth.
Image onscreen:
Jacoby and his parents walk through a wooded park. Jacoby’s dad is holding a travel coffee mug. The video intermittently cuts back to Jacoby’s interview shot before continuing with the walking scene. The family continues to walk through the park and along a small lake, talking with each other and smiling. They walk over to a bench, sit down, and continue talking.
Jacoby:
He makes things really easy to understand. The way that my doctor talks to me makes me feel like this is something that I can handle for the rest of my life, so it’s easier to focus on the things I love, like hockey, football, guitar, and just life.
Julie:
It’s been incredible watching Jacoby learn to advocate for himself. He and his doctor have such a good relationship. He asked questions, he understands what his medication does, and that matters because having the right team, having doctors who listen to him, who respect him, has made all the difference.
Image onscreen:
Julie is seated in an interview chair, talking to at an interviewer off-camera.
Julie:
If I could go back and tell anything to myself when Jacoby was a baby, I would say, “Don't worry, it’s going to be okay.”
Image onscreen:
Jacoby sits in between his parents on the park bench as they continue to talk. His parents then lean in on either side of him and give him a hug. The video fades to white.
Julie:
I would tell other parents to trust your instincts. Push for answers. Surround yourself with doctors who listen and know that NF1-PN is not a roadblock. It's just a different path.
Image onscreen:
The GOMEKLI logo appears large in the center of the screen with disclaimer information in multiple lines along the bottom.
Text onscreen:
©2025 SpringWorks Therapeutics, Inc. All rights reserved. GOMEKLI is a registered trademark of SpringWorks Therapeutics, Inc. SpringWorks Therapeutics, Inc. is a healthcare company of Merck KGaA, Darmstadt, Germany. C_GOM_US_0294 11/25
A presentation about GOMEKLI
Hear more about GOMEKLI treatment from Austin, a Patient Ambassador, and his doctor and learn about free patient support available through SpringWorks CareConnections®.
A purple background featuring headshots of three people. From left to right, the photos are labeled with the names: Dr. Angela Hirbe, Austin, and Tara Herington.
Text onscreen:
See beyond the limits of NF1-PN
Learn about a treatment for adults and children
Image onscreen:
Screen transitions to a presentation slide featuring the headshot of Dr. Hirbe.
Text onscreen:
Chapter 1: An Overview of GOMEKLI
Dr. Angela Hirbe
GOMEKLI study investigator and Austin's doctor; Washington University School of Medicine, St. Louis
[Dr. Hirbe]
Welcome, everybody. We're excited to have you here today. My name is Angie Hirbe and I will be one of the presenters today.
The presentation is sponsored by SpringWorks Therapeutics. And they're committed to developing therapies for patients with rare diseases. So, very happy to deliver this much-needed treatment option, GOMEKLI, or mirdametinib.
GOMEKLI is the first FDA-approved treatment for both adults and children with NF1 plexiform neurofibromas. I will give an overview of GOMEKLI and kind of talk about some of the clinical trial data as well as dosing and administration.
And then I'll hand things over to our GOMEKLI patient ambassador, Austin, who's one of our patients. He'll talk about his experience with living with NF1-PN and being on GOMEKLI. And then, finally, Tara will talk about the SpringWorks CareConnections® patient support program.
So we will get started.
So first, I'm just kind of going to go over some of the safety information and I'll talk a little bit about it more later. But just, you know, very brief overview.
You know, before taking GOMEKLI then you need to obviously talk to your physician about any conditions that you have, but especially if there are any eye problems, heart problems, or thoughts about becoming pregnant because there can obviously be side effects to any medication for an unborn baby.
So again, there's information here. For females, if you're going to become pregnant, then obviously again, you want to talk to your physician first.
And then it's also very important to talk to your healthcare provider about any medications that you take, and that includes prescription medications as well as over-the-counter medications, because all of these things can have drug interactions.
And so we as providers need to be aware of that so we can make sure that the medication is safe.
Again, possible side effects. And I'll go into some of this later on too, when talking about the clinical trial data.
But, you know, we worry about a couple serious side effects that are not common, but certainly serious. And so you need to be aware of these things.
So eye problems are one. Anytime you know, you would experience any blurry vision, loss of vision, changes in vision that needs to be reported to your physician right away.
Heart problems. We know that GOMEKLI has, or any MEK inhibitor has, been shown to potentially decrease the pumping function of the heart, something we call the ejection fraction. And so, it's very common for us to get an echocardiogram as a special ultrasound of the heart. So we know what the pumping function is at baseline. And then we monitor that pumping function throughout treatment with the medication.
So side effects that you worry about that would alert you to that are things like coughing, shortness of breath, fluid, swelling. So swelling in your feet or your ankles, or increase in heart rate. And then skin problems.
So rashes are actually common with any MEK inhibitor including GOMEKLI. But sometimes these can be severe. So anytime you have any kind of skin changes, that's also something that you should talk to your physician about early. We always like to treat things early before they become a big problem.
So what is an NF1 plexiform neurofibroma? So, we know that NF1 is a genetic condition.
It's actually the most common tumor predisposition syndrome, and it affects about one in 2500 people worldwide. Plexiform neurofibromas are tumors that can form in in patients with NF1 and about 50% of patients with NF1 will develop these plexiform neurofibromas. And these are different from other neurofibromas.
So plexiform neurofibromas are, they tend to be bigger tumors.
And they arise from multiple nerve roots. So these are different than the cutaneous neurofibromas that are on the skin or the subcutaneous neurofibromas that are right under the skin.
So what are the most common symptoms of NF1 plexiform neurofibromas?
And so, you know, the things that, you know, our patients will notice the most are pain, difficulty moving around, sometimes because of the location of the tumor and how bulky it is, sometimes because of pain or changes in appearance.
So some of the larger tumors, can obviously be disfiguring or, you know, can make things like wearing clothes difficult, depending on the bulkiness of the tumors.
But they can also impact things like vision, hearing, or breathing depending on where they are.
And we know that 85% of these tumors cannot be completely removed by surgery. And often when patients have debulking surgeries, unfortunately, the tumors will grow back. So GOMEKLI or mirdametinib is the first FDA-approved medication proven to shrink plexiforms in both adults and children with NF1 plexiform neurofibromas.
And this drug is something called a MEK inhibitor.
So this is a targeted drug meaning it's kind of going after one specific pathway in a tumor cell, not a traditional chemotherapy, where I think of chemotherapy as like big guns that are just going after, you know, rapidly growing cells and have lots and lots of side effects.
The MEK inhibitor, you know, we know with patients with NF1, you have a mutation or loss of that NF1 gene. And NF1 is something that's an important stop sign in our cells.
So it tells them to stop growing.
And so the MEK inhibitor, while we can't replace NF1 it kind of helps to put a stop sign back into the cells to help to tell them to stop growing.
So I'm going to go over some of the data from the clinical trial.
So GOMEKLI was studied in one of the largest clinical trials for NF1 plexiform neurofibromas. So this was a single-arm trial that included 114 patients with NF1 plexiform neurofibromas.
So there were 58 adults. So those are patients over the age of 18 and then 56 children. So those are kiddos from the age range of 2 to 17.
And at the start of the trial, pain and changes in appearance were really the most common plexiform neurofibroma-related symptoms that were reported. So before enrolling in the trial, 69% of adults and 36% of children and adolescents had tried surgery to remove their plexiform neurofibromas before.
So again, this is the first treatment proven to shrink tumors in both well, really in adults with plexiform neurofibromas, it’s the first.
So if you look at this slide here, so 41% of adult patients, so that’s 24 out of 58 that were treated with GOMEKLI had their plexiform neurofibromas shrink by at least 20%.
And so the little circles are supposed to give you kind of some guide to see, what is 20% shrinkage?
So if you think of that circle as a plexiform neurofibroma before starting GOMEKLI, being 20% smaller would make the circle look like that.
And then of those patients who had their tumor shrink, 15 of them really saw their plexiform shrink by more than 50%.
And so, again, drawing your attention to the next circle on there kind of shows you what is 50% smaller if we're pretending the plexiform is a perfect circle.
And that reduction in plexiform neurofibroma size was confirmed on later MRI or magnetic resonance imaging scans.
And that 50% reduction was something that we call an exploratory analysis meaning it wasn't specifically designed in advance in the protocol.
The real endpoint was that 20% smaller. So in adults who benefited from GOMEKLI, the plexiform started to shrink within months, not weeks.
So we tried to set the appropriate expectation for patients. So, these these drugs don't have an effect immediately.
But if we look at the data by about four months, 46% of the patients saw results, and then by 12 months, 71%.
So 17 out of the 24 that that had shrinkage saw results.
So if we think about that age range, or the range in which that happens.
So when adults that benefited from treatment, plexiforms began to shrink by at least 20%, for some patients by four months.
But the range is pretty big.
So some patients didn't see that effect until being on the medicine for 19 months, and then the median or the middle amount of time that it took for the plexiforms to begin shrinking was 7.8 months.
So you need to think about that when you're starting therapy, that it may take a while before you see a benefit.
So, it's one of the reasons why we try to work really hard to make the side effects manageable so that we can know whether or not a patient has a benefit from the medication.
And the clinical trial was for two years long, and after that, 84% of adults chose to keep taking the medication in an optional long-term follow-up portion of the study. So again, the medication has also been proven to shrink plexiforms in children and adolescents with NF1 plexiform neurofibromas.
So 52% of the children, so that's 29 out of 56 saw their tumors shrink by at least 20%.
And so again, I have the circles here so you can remember, what does 20% look like?
And then 15 of those children saw their plexiform neurofibromas shrink by more than 50%.
So again, 50% smaller if we're pretending these are perfect circles.
And again these were confirmed on later imaging scans. And then the time frame for expecting a response is similar in the children as it is in the adults.
So again 45%.
So 13 out of 29 of the patients saw results after four months on therapy, and 83%, so it’s 24 out of the 29 patients saw results by about a year.
And that middle time point, you know, the median amount of time that it takes for the plexiforms to shrink was the same in kiddos. So about 7.9 months.
And again that range is 4 to 19 months. So it may take some time before patients see a response.
So it may take some time before patients see a response.
So kind of going through, what are the most common side effects that we see?
The most common things that we see in adults and children are diarrhea. And that does respond pretty well to Imodium, nausea, sometimes some muscle or joint pain, and then vomiting.
Adults also tended to complain of some tiredness or fatigue.
And children and adolescents, the sort of more common things that we saw are sometimes just stomachaches, so abdominal pain, headaches.
And then the rash that you see in children and adults is a little bit different.
So in adults, we see more of this acne-like rash, and kiddos, it tended to be, sometimes just some skin redness and then something called a paronychia, which is where you get this swelling or pain around the fingernails or the toes.
And then one of the most common lab abnormalities that we see is an elevation in something called CPK.
And this is an enzyme and it's in your muscles and, so sometimes, you know, we would see an increase in this lab test.
And most often, you know, it doesn't mean anything and patients don’t have any symptoms but it is something that we do need to keep an eye on.
Because if it gets super high, sometimes that protein can clog the kidneys, and that can cause problems.
But actually having a problem, you know, from this lab abnormality was exceedingly uncommon in the trial.
And then some children also experience a decrease in their white blood cell count, specifically the neutrophils.
And these are cells that are important to fight infection. But despite that lab abnormality, there weren't, you know, increased infections or anything like that in the kiddos.
And then again, the serious side effects.
So the eye problems, we always want to know if a patient has any vision changes, and we do make sure that patients get their vision monitored during treatment.
Heart problems, we talked about before. These medications can affect the pumping function of the heart. So it's something that we keep a close eye on.
And then skin problems.
Rashes are pretty common in kids and adults, so the rash is different in children versus adults.
And most of the time the rashes are not serious, but they can be.
So it's important to talk about things up front, so that they can be addressed.
So among adults, about 22% of patients did stop treatment due to a side effect.
That number was smaller in children, so only about 9% stopped treatment due to a side effect.
And then if we look, what do these pills look like and how are they taken?
GOMEKLI comes in two different forms. So there is a grape-flavored tablet that you can make an oral suspension with.
So that can dissolve in liquid.
And so it can be taken that way.
So for younger children who can't swallow pills, or even for some adult patients who may have difficulty swallowing pills, that is an option for patients.
And then there's also capsules that come in two different sizes, so a 1-mg smaller capsule and then a 2-mg capsule.
The medication is taken by mouth, you know, twice a day, so about 12 hours apart.
It can be taken with or without food. And then again we look at side effects in terms of, you know, deciding whether or not a patient is benefiting and should stay on medication.
So there's also a built-in treatment break with GOMEKLI.
So if you look at how the medication is taken, the dosing cycle is 28 days or four weeks, but the actual medication is taken twice a day for the first three weeks, or 21 days.
And then, you get seven days where the medication is not taken, so that's that treatment-free week, and then the cycle starts over again.
So I will stop there and turn it over to Austin.
Image onscreen:
Screen transitions to a presentation slide featuring the headshot of Austin.
Text onscreen:
Chapter 2: My GOMEKLI story
Austin
GOMEKLI Patient Ambassador; currently on treatment
[Austin]
Hello! My name is Austin. I'd like to thank SpringWorks Therapeutics for sponsoring me for me to share my story with you all here today about living with neurofibromatosis type 1 with plexiform neurofibromas or NF1-PNs, and being treated with GOMEKLI or mirdametinib.
So when I was two and a half years old, my parents noticed a large discoloration on my back that resembled a bruise like, at first they just thought it was, they thought it was a bruise.
I have a brother that's 11 months older than me, and they thought my brother sat on me. You know how boys will be boys. But after it didn't go away for a few weeks, they grew some more concerns.
And, they took me to the doctor, and I -- we found out it was a tumor. My father and paternal grandmother both have neurofibromatosis type 1. We were kind of worried that I would have a predisposition of being able to get that.
Because of this my family is always aware of the possibility of NF1 being passed on to me.
While they had some understanding of NF1, they weren’t really prepared for exactly how serious this was.
When we learned that that bruise was a tumor, I went in for a lot of testing. I was much too young to remember exactly what everything we did. But when I was diagnosed with that plexiform, from that point on, my life totally changed.
Especially in my toddler years when I was going to a lot of doctor visits, being monitored, dealing with a lot of back pain. And we even actually ended up giving my tumor a nickname, “Ralph, the runaway mouse,” after the old children's book that I loved. So my doctors warned my parents that the tumor could grow. And if it did grow, I would more than likely have to undergo surgery to remove part of it or debulk it, which was high risk due to several complications, especially because it was growing around a lot of key nerves.
Especially the nerves that would help me walk. Lo and behold, the doctors were right and two years later, the tumor was now the size, was now a great a good size. and I would have to have surgery to get it removed.
On February 2nd of 2000, 2/2 of 2000, at four and a half years old, when you know you're a kid, supposed to be learning how to ride a bike, swim, and have fun on the playground, I was undergoing my first major surgery. Only part of the tumor was removed, otherwise it would have paralyzed me from the waist down. The portion of the tumor that was removed was the size of a foam football.
So imagine about a four-year-old kid and a foam football being removed from their back.
It weighed about 20% of my body weight at the time. After that surgery, I was bedridden for quite some time.
And just ten months later, after continuing to be monitoring, we found out that it was growing back into my spine and we had to have a second surgery. This time they removed a portion that was the size of a golf ball. Now you may think I was a little too young to understand everything that was happening to me, but both my parents were in the first-responder field.
My father was a firefighter/EMT, and my mother was a nurse. They taught me the importance of self-advocation even at such a young age. Doctors would want to pull my parents out of the room and talk to me about the seriousness of what was going on and making these key decisions, and they would flat out tell them, “No, Austin has to live with this his entire life. He needs to be part of these decisions to know what's going on."
And especially because now I had that giant scar and you could see my tumor.
You know, other kids would see it at the pool or something and I could just explain to them.
With this, I also had many limitations.
My memories growing up included a lot of sitting on the sidelines of playing sports or on the playground when kids would run around having fun, including my older brother and my younger sister. My pain was very unpredictable. When I could try to participate at times, and I would, but then I'd have to go sit down because of how bad my back would start to hurt, and I would sometimes just lie down in the grass.
At school, I tried my best to fit in with my peers and participate in gym or outside at recess, but it didn't always work out right.
When most kids would play sports or did some fun extracurricular activities, I wasn't able to do much of those.
Between my severe pain, the doctor's appointments, and just everything that was going on, I struggled. And this also kind of struggled to help me focus on my studies at times as well, let alone even have a social life.
The worst part was growing up with two siblings who didn't have the same limitations as me. I couldn't help feeling left out at times because they were able to do everything at a more advanced pace than I could.
I was living a completely different life from them. It was a battle to try to get them to understand that I wasn't lazy, or that I didn't want to do something, it's just that I couldn't do something.
And this even went on into my school years with teachers or, you know, friends’ parents as well. But even from the sidelines, I was always teaching others about my NF1-PNs.
My parents said that if someone made fun of me, I should use that opportunity to educate them because them poking fun or making fun of me was them just the lack of them understanding.
So as I grew up, my pain levels would vary.
There were times when my pain was uncontrollable, where I could barely move or get out of bed, or to where I would be in the hospital for several weeks in pain. I saw several doctors, including pediatricians, pain management doctors, and NF specialists. We would try over-the-counter pain medications to help manage my pain, but it didn't always work.
And by the time I was 18, however, I kind of had a new tide. I was in a little bit less pain, so I thought it all was doing a lot better.
I decided to take a break because I was tired of seeing doctors all the time and going to appointments and medical treatments and all that, and I was 18.
I was an adult now. I thought I can make my own decisions and I just wanted to feel free and normal for a change. So after graduating high school, no longer dealing with that, I decided to chase one of my biggest dreams.
Like my parents dedication to serve others in their career, I was determined to join the military. Unfortunately, with my tumors, I could not join the military. So I did the next best thing and I went into a law enforcement career.
I tried my best to get through that. I could not advance in my career because of my pain, but I didn't let it stop me from at least trying and helping others along my way.
I started off in corrections, then I moved up to be a deputy sheriff, where I was a bailiff, and then I became a public safety officer.
And then things got worse again, where my pain came back full-fledge force.
It was just relentless. I was about 22 years old when that severe pain came back, and it just started where I could barely move, let alone do my job. I knew it was time to see a doctor again.
And with my mobility issues starting to take over, starting to be worse, I was taking more over-the-counter pain medications, so I knew it was the right time.
For six years, I proudly wore my badge, but the pain eventually just became too much and I had to step away from that career.
It was more than just leaving a job for me. It was leaving a calling in something that I had worked hard for.
I knew I couldn't live like this anymore with my severe pain, and as I even struggled to have a job in retail at that point, I think back on it and I do regret my decision to stop seeing my doctor. And I still wonder that if I stopped, if I didn't stop, maybe I could have furthered my career and have less pain in the long run. But that's neither here nor there.
When I got back in to see my doctor, we both agreed it was a good time for me to start treatment for my NF1-PN, so my primary doctor referred me to an oncologist.
So I went to her office, eager and hopeful to start a new journey on my NF1-PN.
And then during the appointment, my oncologist mentioned a clinical trial that was coming up for a medication called mirdametinib, or now, GOMEKLI.
She explained that the goal of the trial was to decrease the tumor size by at least 20% in adults and children two and older. So in about 2020, once we learned that I qualified for the trial, we got started.
I take GOMEKLI twice a day, oral pill, for 21 days, and then I'm off it for seven.
Since starting GOMEKLI I have experienced some of those side effects.
At the start, the side effects seemed a little more worse, but now they're a lot more minimal.
One of the biggest side effects I had was the skin rash, which was almost to me, it seemed more like looked like a, poison ivy. But it wasn't.
And I used baby lotion and it kind of soothed the itching and helped it out. At least that's for me personally. For everybody else, it may be different. And definitely consult your doctor.
So, and then at the one-year mark, after going through all these testings every couple months and to the doctor always, I was kind of tired of it again.
And I seriously considered stopping it just because it was kind of a struggle to get to the doctor all the time and put my life on hold just to do two days' worth of doctor's appointments between the testing and then the doctor.
So I talked to my mom about that, and I told her that I was thinking about it, depending on what the results were, and my mom said it was my decision.
Well, we went to the doctor's office, and we sat down, and when Doctor Hirbe got in there and I was speechless because what she told us was my tumor shrank 57% in the first year.
[applause] Yeah, I, I just could not say a word. And I remember my mom turning to me and just saying, “Well, that answers your question about whether you should stay on the treatment or not.” So that moment marked a turning point for me.
For years I'd seen my NF1-PN as a burden, but hearing that my tumor was actually shrinking, I felt like I had a completely new outlook.
Again, this is just my experience and others' may be different, but it gave me a little more hope in my life that if that could change, what else could change in my life?
My oncologist and I both agreed that GOMEKLI was working, and I would stay on it as a part of a long-term, optional, follow-up phase of the study, and I've now been on it for a little over five years. Through my journey with NF1-PN, I've given up a lot in my life. I had to give up my goal of going into the military, my law enforcement profession.
But I have found a new purpose, one that's allowed me to connect my career to serving people.
One that I thought about doing for a long time as well, I became involved in ministry. I'm a pastor, and I stepped into the role earlier this year as a full time pastor, and it's been one of my proudest achievements, and I'm now thankful to be able to offer guidance and support to others in their lives. The flexibility ...
[applause] Thank you, yeah. And the flexibility of this role has also allowed me to continue my doctor's appointments to help me easily manage my NF1-PN, and also be able to help other people as well.
I now know how important it is to stay on top of my care and continue to monitor my NF1-PNs even when it doesn't seem as severe. I see my oncologist about every three months and my pain management specialists every six months. My oncologist and her team are great.
She's very approachable, easy to talk to, and she's like family. We can joke around when the moment calls for it, but we can also get, shift to serious topics when needed.
One of the most recent examples is I got a bad sunburn on my right arm. I'm not going to hear the end of that. Five minutes.
Yes, five minutes ago. But she's always ready to help me find a solution to any of my problems.
And if she doesn't have an answer for me, she’s always spot on with me with honesty and always will get back with me in a timely manner. Since I've dealt with NF1-PN my entire life, I feel that I'm pretty knowledgeable about it, allowing me to have more advanced conversations around this. Of course, I have my parents to thank for that because at a young age, being able to self-advocate and take charge of my own care.
To own your own care is probably one of the most important things any of us can do with NF1, especially with PNs. I've had to accept my own limitations in life, which are things I tend to challenge maybe a little more than I should. But I do love the outdoors: camping, hunting, hiking, fishing, and unfortunately, not all those activities are easy to do with my NF1-PNs, especially when I have a spike in my pain.
But I've learned to manage the best I can, and go through working with my doctor and taking my medications to be able to afford me more opportunities to partake in the things I love to do.
I often heard patients with NF1-PN use the words “adapt” and “cope,” and that is what SpringWorks Therapeutics researchers have worked to help patients do, and I'm thankful for them. I know what it's like to feel limited, to sit on the sidelines, to struggle with pain and and to miss out on my dreams, but to find new ones.
And that gives you the hope. To anyone struggling with your own NF1-PN journey, you're not alone. Your path may not look the way you imagined, but there's still a future worth fighting for.
And with all of us together behind you, we can do it together. Thank you.
Image onscreen:
Screen transitions to a presentation slide featuring the headshot of Tara Herington.
Text onscreen:
Chapter 3: A Look at SpringWorks CareConnections®
Tara Herington
Executive Director, Global Patient Access at SpringWorks Therapeutics
[Tara Herington]
So I'm here to talk about our SpringWorks CareConnections® support program that supports people who are starting on GOMEKLI or staying on GOMEKLI.
So this is a personalized support program. You'll hear me say “personalized” a lot.
And it's a free program, and it's for insurance navigation. So we all know that can be a little tricky.
There's also financial assistance that we offer.
And we also have personalized educational and emotional support with our nurses.
And so I'll go into each of these three things in more detail.
How many people have really struggled with insurance before? I know I have and just trying to figure things out. So one of the things we do is we have a team that really looks into the benefits, figures out if it's covered, if it's not covered, how much the copay will be, is there any deductible remaining?
Just all of those out-of-pocket costs and figures all that out. And then the next step would also be doing a prior authorization.
Almost always I'll have to say a prior authorization is needed. And then if the prior authorization is denied, then we also have the ability to work through the appeal process.
And we have a lot of tools available for patients and for their HCPs, for their healthcare providers, to support that. And then we also have financial assistance.
The financial assistance, we have a copay, offering a commercial copay offering. It's a $0 copay card. So for the 21-day supply, I always say $0; free is my favorite color.
So we have our copay program.
We also have a program to help because we know it's not just the medication.
There are also other out-of-pocket costs that are associated with being on a medication.
And so we also have coverage for that, for eligible visits, for examinations. It can be a visit to a specialist.
It can be testing...things like that. And so I know your next question is going to be, okay, what are the…what's the eligibility?
So we do have some different criteria.
So it's for residents of the United States or its territories or possessions.
Also this is for the copay program, for the 21-day supply, for the $0.
It's commercially insured. So usually we think of that as if you have insurance through your employer. So not Medicare, not Medicaid, through your employer.
A prescription, of course, for GOMEKLI, a copay greater than zero and then also for that insurance coverage.
If, we do have…sometimes we find folks who still struggle with affordability even after all this, we have other programs, too, that are available to folks.
And the way to know about those is through our the nurse navigators that we have. And I'll go into the Nurse Advocates in just a minute. But there are a couple of QR codes that we have.
So there's one up here.
So, that you'll see there's another one later. So if you get your phones out and want to take advantage of that, I just want to make sure that you're ready.
So our Nurse Advocates were designed to be a single point of contact to work with people who are starting on or staying on GOMEKLI and their family members or loved ones.
And so this is the person that you'll meet, when first being enrolled in the program, and they work with folks from the very beginning all the way through.
And this could be anything with, you know, like how to take the medication as prescribed. They're all trained in NF1-PN, and of course, they're all trained on GOMEKLI. Many had experience with NF1-PN prior to joining our program.
So they also could answer questions about disease state, things about managing treatment over time.
Sometimes people have, oh gosh, maybe they're starting a new job, and they have new insurance and they want to know how will this work with my new insurance?
Will I still be able to stay on GOMEKLI? So they can help through that.
And then also help plan conversations with the care team.
When the patients and the Nurse Advocates are talking together, the Nurse Advocate may say, “Hey, that's a great point to bring up with your doctor. Make sure you write that down so you have it during the next visit.” So they really are there all the way through, every step of the way.
And then we also have something new that we just brought out really recently and we're excited about it, and this is our Digital Companion.
So you may be familiar with Medisafe. We've partnered with Medisafe. Medisafe is a, it's a health tracker, a really robust health tracker. I know I like to use it for keeping things like, you know, all the different doctor's appointments I may have, things like, just lab results.
It just keeps everything right there in your phone, which we always have with us all the time. And then we've created some customized support through the Medisafe app that's specific to GOMEKLI.
So that means there are specific medication reminders for the three weeks on, the one week off.
We also have access to educational content that's specific to GOMEKLI.
You could even reach out and, reach out to your Nurse Advocate through the Digital Companion. So it's a really nice offering for folks who are taking GOMEKLI.
And so, with that I’d like to, on behalf of SpringWorks, really thank you for your attention today. You've been great. Thank you so much to Doctor Hirbe and to Austin for sharing your story. That was that was great. You can also go to GOMEKLI.com to get more information.
Image onscreen:
Photo of a couple dancing to a live band appears alongside a QR code to GOMEKLI.com.
Text onscreen:
Thank you!
Learn more at GOMEKLI.com
Image onscreen:
SpringWorks logo and GOMEKLI logo appear.
Text onscreen:
©2025 SpringWorks Therapeutics, Inc. All rights reserved. GOMEKLI and SpringWorks CareConnections are registered trademarks of SpringWorks Therapeutics, Inc. All other trademarks and logos are property of their respective owners. C_GOM_US_0428 8/25

Meet Austin

Meet Julie and Jacoby

A presentation about GOMEKLI
Downloadable tools and more
A variety of helpful resources to support you throughout GOMEKLI treatment.
NF1-PN=neurofibromatosis type 1 with plexiform neurofibromas.
What is GOMEKLI?
It is not known if GOMEKLI is safe and effective in children under 2 years of age.
Important Safety Information
Before taking GOMEKLI, tell your healthcare provider about all of your medical conditions, including if you:
- Have eye problems
- Have heart problems
- Are pregnant or plan to become pregnant. GOMEKLI can harm your unborn baby
Females who are able to become pregnant:
- Your healthcare provider should check to see if you are pregnant before you begin treatment with GOMEKLI.
- Use effective birth control (contraception) during treatment with GOMEKLI and for 6 weeks after your last dose.
- Tell your healthcare provider right away if you become pregnant or think you may be pregnant during treatment with GOMEKLI.
Males with female partners who are able to become pregnant:
- Use effective birth control (contraception) during treatment with GOMEKLI and for 3 months after your last dose.
- Tell your healthcare provider right away if your female partner becomes pregnant or thinks she may be pregnant during treatment with GOMEKLI.
- Are breastfeeding or plan to breastfeed. It is not known if GOMEKLI passes into your breastmilk.
- Do not breastfeed during treatment with GOMEKLI and for 1 week after your last dose.
- Talk to your healthcare provider about the best way to feed your baby during this time.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
How should I take GOMEKLI?
- Take GOMEKLI exactly as your healthcare provider tells you to take it. Your healthcare provider may change your dose, temporarily stop, or permanently stop treatment with GOMEKLI if you develop certain side effects.
- Take GOMEKLI twice a day, about 12 hours apart, for 21 days, followed by 7 days off treatment, to complete a 28-day treatment cycle. Your healthcare provider will decide how many treatment cycles are right for you.
- Take GOMEKLI with or without food.
- GOMEKLI comes in two different dosage forms, GOMEKLI capsules and GOMEKLI tablets for oral suspension. Your healthcare provider will decide the dosage form and dose of GOMEKLI that is right for you.
- If you take GOMEKLI capsules: Swallow each capsule whole with drinking water. If more than 1 capsule is required, swallow 1 capsule at a time. Do not open, break or chew the capsules.
- If you take GOMEKLI tablets for oral suspension, either:
- Swallow each tablet for oral suspension whole with drinking water. If more than 1 tablet is required, swallow 1 tablet at a time.
OR
- Disperse the tablets for oral suspension in drinking water to make a liquid (suspension) before you take or give GOMEKLI.
See the “Instructions for Use” that come with your medicine for instructions on how to prepare and take GOMEKLI tablets for oral suspension.
What are the possible side effects of GOMEKLI?
- Eye problems. GOMEKLI may cause eye problems that can lead to blindness. Your healthcare provider will check your vision before and during treatment with GOMEKLI. Tell your healthcare provider right away if you get any of the following signs or symptoms of eye problems:
- Blurred vision
- Loss of vision
- Other changes to your vision
- Heart problems. GOMEKLI may lower the amount of blood pumped by your heart, which is common in children during treatment with GOMEKLI and can also be severe. Your healthcare provider will do tests before you start GOMEKLI treatment, every 3 months during your first year of treatment, and then as needed to make sure your heart is working properly. Tell your healthcare provider right away if you get any of the following signs or symptoms of heart problems:
- Coughing or wheezing
- Shortness of breath
- Swelling of your ankles and feet
- Tiredness
- Increased heart rate
- Skin problems. Skin rashes are common with GOMEKLI in both adults and children and can also be severe. GOMEKLI can also cause hair loss (alopecia). Tell your healthcare provider if you develop any of the following signs or symptoms of skin problems:
- Flat skin rash
- Raised bumps on the skin
- Skin bumps that look like acne
- Skin redness
- Itchy rash
- Peeling skin
The most common side effects of GOMEKLI in adults include:
- Diarrhea
- Nausea
- Muscle, joint, and bone pain
- Vomiting
- Tiredness
The most common side effects of GOMEKLI in children include:
- Diarrhea
- Muscle, joint, and bone pain
- Stomach (abdominal) pain
- Vomiting
- Headache
- Skin redness, swelling, or pain around the fingernails or toenails
- Nausea
What is GOMEKLI?
It is not known if GOMEKLI is safe and effective in children under 2 years of age.